October 11, 2015. It was close to 12:30 A.M. and we had been asleep for less than an hour when Dad started coughing. After 90 minutes of his intermittent hard coughing, Dianne convinced him to use the Yankauer wand attached to the suction machine to remove some of his own secretions. Within a few minutes after using the wand, Dad was sleeping. Dianne also went back to sleep, but at 4:15 A.M., something woke her. To her horror, Dad was on his knees on the floor. He needed to use the bathroom and for some reason, he thought that he could get there by himself. In a panic, Dianne paged me through the baby monitor. The anxiousness in her voice propelled me out of bed and down the stairs. The two of us tried for a few minutes, but we could not get him off of the floor and back into the bed. Fortunately, my husband was in town. I called for Stan through the baby monitor, and the three of us were able to get Dad off of the floor. At 4:50 A.M. we finally had him back in the bed. Once again, he was lucky that he hadn’t hurt himself. I could only suppose that when he woke up at night he couldn’t remember that he couldn’t walk or that he was hooked up to two devices. Depending on how he might fall, he could put a strain on his trach and decannulate himself or pull out his G-tube. Just the thought of such things happening gave me the heebie-jeebies.
I woke up again at 6:45 A.M. and woke Dianne and Dad. Dianne and I assisted Dad into his wheelchair and he wheeled himself into the master bathroom to wash his face, brush his teeth, and shave. Dianne gave him a sponge bath and helped him get dressed. He might have needed a few days to reacclimate himself to his house, but after 148 days in a hospital gown, he knew what he wanted to wear and told her where to find it. When he was all shiny and dressed, I stopped by his room and administered his trach care and morning meds. When I was finished, Dianne and I reattached his humidified oxygen and tube feed.
After breakfast, Mom shooed Dad out of the master bath and I went upstairs, and the two of us got ready for church. As we drove to church, I updated Mom on the activities of the previous night. We both enjoyed our respite at church and then returned home to an empty house, although there were two cars in the garage and three cars parked out back.
It was another beautiful day and shortly after Mom and I had left for church, Dad told Dianne that he wanted to go outside. She pushed him outside and she helped him navigate his wheelchair over the entire backyard. My parents’ house sits on an acre lot, so Dad had a lot to show her. After being out in the sun for 40 minutes, they moved to the patio and sat in the shade. Under the best of circumstances, spraying the trach bib provided only a modicum of moisture. Although Diane did her best to keep Dad’s trach bib wet with the spray bottle of sterilized water, the outside air was very dry, so he was breathing in a lot of dry air. After finding them on the patio, I became a little agitated that he had been off of the humidified air for a couple of hours. After a bit of foot-tapping from me, Dad agreed to come back inside.
Just a short time later, Dad said that he needed to go to the workshop in the garage to find a tool for Stan. It was 99 degrees outside and still dry. After he had spent 10 minutes in the workshop with Stan, I insisted that he go to his room for humidified air and nutrition. I kept pestering him to come inside, but he was uncooperative and became angry at my repeated attempts to get him back indoors. I was exasperated. I tried to explain that any time that he spent outdoors was time that he breathed dry air into his lungs and deprived his body of nutrition, yet I was the bad guy.
Finally, at 4:15 P.M. we finally got him back in bed and hooked up to his essential lines, and he quickly drifted off to sleep. Before Dad closed his eyes, Stan came to his room to say goodbye. Stan was returning to Houston but would come back next weekend.
Dad slept until 6:00 P.M., at which time we had happy hour. Sometimes he would sit and talk with us during happy hour, but today he spent most of the time wheeling himself around the house. I can’t begin to imagine how difficult it would be to not be able to sip a drink or eat my favorite foods, and sometimes it seemed that the denial of one of life’s pleasures depressed him. When Mom announced that dinner was ready, Dad wheeled himself back to his room. Dianne trailed after him and helped him back into bed and attached him to the tube feed and humidified air.
By 7:00 P.M., we had the dining room table cleared and the dishes in the dishwasher. We helped Dad back into his wheelchair and we played another cutthroat game of Oh Hell.
Tomorrow would be a work day for me, so I was glad when we started getting Dad ready for bed at 8:45 P.M. Truth be told, it was still past my bedtime. Dianne helped Dad get ready for bed and I administered the nighttime meds and trach care. After I left the room, Dianne coached Dad through his exercises prescribed by the physical therapist.
He had had a full and busy day, and he fell asleep as soon as he finished his exercises. His coughing briefly woke him up at 11:00 P.M.
October 12. Dad slept pretty well until 1:00 A.M., at which time he started coughing again. Again, Dianne convinced him to use the Yankauer wand and suction machine to clear out some of his secretions. He didn’t sleep much afterward and was very restless. I could hear his coughing and gurgly breathing through the baby monitor, and at 3:00 A.M., I got up, donned my scrubs, and suctioned secretions from his trach. When I was finished, Dad assumed that it was time to get up. I explained to him that it was Monday and that he didn’t need to get up early for dialysis, and he agreed to go back to sleep.
After I cleaned up the trach-cleaning supplies, I went to my parents’ office and logged on to work. For about three hours, I was the only one who was awake. Although I was on Skype almost nonstop, my talking didn’t disturb Dianne or Dad. In addition to Dad being hard of hearing, the oxygen generator was noisy and blocked all sound outside of the master bedroom. My mother was sleeping in a room on the opposite side of the house. I could crash cymbals and not wake up anybody.
At 6:30 A.M., the residents of the master suite started stirring. Dianne unplugged Dad from the oxygen and the Kangaroo pump and helped him into his wheelchair. Once he was situated, he could wheel himself into the master bath and wash up and shave. Before helping him get dressed, Dianne checked his blood pressure and oxygen saturation. His blood pressure was good, but his oxygen saturation was still hovering in the low 90s. I administered his morning meds and trach care and went back to work.
While Dianne got ready for the day and ate breakfast, Dad sat in his room, received humidified air and nutrition, and read the newspaper. At 9:00 A.M., he was ready to go outside and have Dianne help him with some yard work. When he said he wanted her help, he meant that he would tell her what to do. I told him that our aides were not here to do his yard work. Dianne interrupted, insisting that she would love to go outside and do some light yard work. I shook my head and headed back to work while Dianne wheeled Dad outdoors.
Dad and Dianne stayed outside for about an hour, at which time I urged them to come back inside for air and nutrition. I couldn’t decide whether I was starting to feel like a broken record or a nag. Dad grudgingly came back indoors and let Dianne reattach him to his humidified air and tube feed. He fell asleep and slept until 11:30 A.M. We were expecting the nurse this afternoon and I wanted to be sure to administer his trach care and change his dressing before she arrived. When I reached to pull off the speaking valve, it wouldn’t budge. I. Could. Not. Believe. It. It was déjà vu all over again. My only consolation was that the nurse would be here soon. I decided to hold off on changing the trach until she arrived; perhaps she might have better luck removing it.
Like an answer my prayers, the nurse was able to remove the speaking valve, and without any muss or fuss. Before she left, she gave me some tips for handling the speaking valve. As the nurse was walking out to her car, the physical therapist aide entered the driveway. Dianne watched the physical therapy session so that she’d be able to assist Dad with his daily exercises. Shortly after the therapist left, Dianne and Dad went back outside. After about 15 minutes, I was pestering them to come back indoors. Dad agreed and Dianne hooked him back up to his air and tube feed.
At 5:10 P.M., I was finished working for the day and was ready for our happy hour. At that moment, Dad and Dianne went back outside for 10 minutes. I couldn’t believe how much time he was spending outdoors. Mom, Dianne, and I were ready for dinner by 6:30 P.M., which enabled Dad to spend some time on the humidified oxygen and tube feed.
After dinner, we played another rip-roaring game of Oh Hell. Although the game can be challenging, it’s even more challenging when you don’t deal the cards correctly—something that seemed to happen often with Dad’s impaired dexterity. Dianne and I started getting him ready for bed at 8:45 P.M. After Dianne helped him to get ready for bed, I administered his nighttime meds and trach care and sat with him while Dianne prepared herself for bed. At 9:15 P.M., I finally dragged myself upstairs to bed, called Stan, set my alarm for 3:30 A.M., and fell asleep.
October 13. With the exception of a little coughing around 12:30 A.M., Dad slept through the night until I woke him and Dianne at 4:20 A.M. As I returned to work, they resumed their morning routine in preparation for dialysis. When they were finished, Dianne dashed to the kitchen to grab a quick bite of breakfast and I returned to the master bedroom and administered Dad’s Midodrine and trach care. The Scott & White ambulance arrived about 15 minutes early, but Dad was ready. Dianne drove her car and followed the ambulance to the dialysis center. The good thing about being picked up at 6:00 A.M. is that, if you’re lucky, your dialysis session will start earlier, which is what happened today.
The aides at One on One Personal Care switched out on Tuesdays, which was a little difficult logistically with Dad’s dialysis. Gale arrived at the dialysis center at 10:30 A.M. and found Dianne and Dad just as Dad’s session was ending. Dianne drove back to the house, picked up her belongings and paycheck, and drove to her next assignment. The aides worked every other week and rest during the alternate weeks. To accommodate our dire predicament, she sacrificed three days of her week off. Gale stayed with Dad until he was picked up by the ambulance and then drove to our house.

It was good to see Gale again. She looked refreshed but confessed that she had been dog tired when she left us a week earlier. During her first night home, when her husband got out of bed to use the bathroom, she bolted up in bed and said, “Where do you think you’re going?” It took her a couple of days home to wind down.
Gale marveled at the change in Dad and said that he seemed much stronger in just one week. A week earlier, it took considerable effort from the two of us to transfer him from the bed to his wheelchair or to the bedside commode. Now she could transfer him with only a little assistance from me.
Dad spent most of the day resting, which meant that he had a few uninterrupted hours of humidified air and nutrition. At 5:00 P.M., we got him up for happy hour and then he returned to his room while Mom, Gale, and I ate dinner. Although she hadn’t won a game yet, Gale was now a pro at Oh Hell. Dad still had a difficult time dealing cards and our cardinal rule was to always count our cards before starting to play a hand.
We breezed through our nighttime routine. After Gale helped Dad get ready for bed, I administered his meds and trach care while Gale got herself ready for bed. When she returned to the room at 8:45 P.M., I retired to my bedroom, set my alarm, called Stan, and hoped for another few hours of uninterrupted sleep.
We quickly drifted back into our routine. Dad and Gale were both kidders, and they resumed their friendly banter.
I couldn’t believe the difference in this day and Gale’s first day with us. I was still constantly on pins and needles and worried that something could go wrong at any minute, but at least we acted like we knew what we were doing.

 His dialysis session was happily uneventful, with no extra bleeding or trips to the hospital. To top it off, the ambulance was on time for the return trip, and Dad and Amanda arrived back home at 11:35 A.M., which was record time.
His dialysis session was happily uneventful, with no extra bleeding or trips to the hospital. To top it off, the ambulance was on time for the return trip, and Dad and Amanda arrived back home at 11:35 A.M., which was record time. Although Dad seemed to like her, I wasn’t enamored with Amanda, and having a new aide would cause multiple interruptions in my work day to train another person. When the doorbell interrupted my pity party, my first thought was that I wasn’t in the mood for company, but I was relieved to see that we had just received a package from Amazon.com. Dad’s padded commode seat cushion had just arrived. The cushion was four inches thick and appeared as if it would have satisfied that
Although Dad seemed to like her, I wasn’t enamored with Amanda, and having a new aide would cause multiple interruptions in my work day to train another person. When the doorbell interrupted my pity party, my first thought was that I wasn’t in the mood for company, but I was relieved to see that we had just received a package from Amazon.com. Dad’s padded commode seat cushion had just arrived. The cushion was four inches thick and appeared as if it would have satisfied that 
 commode that we kept in the common area of the bathroom. Having it in a more open area enabled the aides to transport him to and from the commode, a contraption that he loathed. After helping him into the bathroom to use the dreaded bedside commode, Gale and I were able to convince him to go back to bed. Thankfully, he remained in bed until 8:30 A.M., at which time I administered his trach care and morning meds. I was still a rookie with the trach care and the process took about 45 minutes.
commode that we kept in the common area of the bathroom. Having it in a more open area enabled the aides to transport him to and from the commode, a contraption that he loathed. After helping him into the bathroom to use the dreaded bedside commode, Gale and I were able to convince him to go back to bed. Thankfully, he remained in bed until 8:30 A.M., at which time I administered his trach care and morning meds. I was still a rookie with the trach care and the process took about 45 minutes. also needed to bring a blanket, a box of tissues, and various other items. Gale told Stan that instead of Mom’s Elizabeth Arden tote bag that we were using to transport his dialysis accessories, Dad needed something larger and more masculine, like a duffle bag. Stan wasn’t sure what she had in mind, but he eventually found a gym bag that she deemed perfect for the task.
also needed to bring a blanket, a box of tissues, and various other items. Gale told Stan that instead of Mom’s Elizabeth Arden tote bag that we were using to transport his dialysis accessories, Dad needed something larger and more masculine, like a duffle bag. Stan wasn’t sure what she had in mind, but he eventually found a gym bag that she deemed perfect for the task. During dialysis, Dad used oxygen tanks from the dialysis center, but this service did not include the moisture that he needed to keep his trach moist. In an attempt to compensate for the lack of moisture, Timothy from American HomePatient had provided us with several bibs composed of a porous non-woven material. The bib was placed between the trach and the oxygen source. The bib wouldn’t stay moist for more than 30 minutes, so we kept a small spray bottle in his dialysis bag, and Gale was vigilant about keeping the bib wet.
During dialysis, Dad used oxygen tanks from the dialysis center, but this service did not include the moisture that he needed to keep his trach moist. In an attempt to compensate for the lack of moisture, Timothy from American HomePatient had provided us with several bibs composed of a porous non-woven material. The bib was placed between the trach and the oxygen source. The bib wouldn’t stay moist for more than 30 minutes, so we kept a small spray bottle in his dialysis bag, and Gale was vigilant about keeping the bib wet.

 I returned home from the pharmacy just after 5:00 P.M. and the guys from
I returned home from the pharmacy just after 5:00 P.M. and the guys from 
 After Jennifer left the room, Dad asked me about “all of the buildings that he was going to travel through.” I explained to him that to get home, he wouldn’t travel through buildings, but that his ambulance would take him home via the Loop and 31st Street. I drew him a bad, oversimplified map of the area and explained where everything was and the distances between them. He had been hospitalized so long that he was confused, thinking that there was a difference between our house and our home. He then told me that it would be prudent to get him a bedpan, so I called the nurse and left his room.
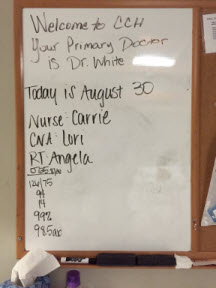
After Jennifer left the room, Dad asked me about “all of the buildings that he was going to travel through.” I explained to him that to get home, he wouldn’t travel through buildings, but that his ambulance would take him home via the Loop and 31st Street. I drew him a bad, oversimplified map of the area and explained where everything was and the distances between them. He had been hospitalized so long that he was confused, thinking that there was a difference between our house and our home. He then told me that it would be prudent to get him a bedpan, so I called the nurse and left his room. At 11:00 A.M., Angela returned, and my respiratory therapy training ratcheted up a notch. In addition to suctioning Dad today, she said that I would
At 11:00 A.M., Angela returned, and my respiratory therapy training ratcheted up a notch. In addition to suctioning Dad today, she said that I would  While I was sitting with Dad, Angela returned to the room with printed instructions about how to suction and change out a trach. Dad was sleeping, so I decided to read the entire document. I write technical documentation for a living, and although I’m not diligent about always reading it, this seemed like a good time to read the manual. I was glad that I did. When Angela stopped by again, I told her that the two other respiratory therapists had had me insert the tubing much further into Dad’s trach than the instructions advised. She told me that she had noticed that I had performed deep suctioning on Dad, but that it wasn’t necessary. When I changed my suctioning technique, I found that suctioning didn’t hurt Dad the way it did with some of the respiratory therapists. I was glad that Angela was now my trainer. I recalled how Dad had told her that she was different from the other respiratory therapists and how he didn’t like others, like Victor. Angela had me suction Dad the rest of the day, and by the end of the day, I was somewhat comfortable with the procedure, although I still had to psych myself up for it.
While I was sitting with Dad, Angela returned to the room with printed instructions about how to suction and change out a trach. Dad was sleeping, so I decided to read the entire document. I write technical documentation for a living, and although I’m not diligent about always reading it, this seemed like a good time to read the manual. I was glad that I did. When Angela stopped by again, I told her that the two other respiratory therapists had had me insert the tubing much further into Dad’s trach than the instructions advised. She told me that she had noticed that I had performed deep suctioning on Dad, but that it wasn’t necessary. When I changed my suctioning technique, I found that suctioning didn’t hurt Dad the way it did with some of the respiratory therapists. I was glad that Angela was now my trainer. I recalled how Dad had told her that she was different from the other respiratory therapists and how he didn’t like others, like Victor. Angela had me suction Dad the rest of the day, and by the end of the day, I was somewhat comfortable with the procedure, although I still had to psych myself up for it. If you spend any time at a hospital, you quickly learn that healthcare is a dirty business and the floor is difficult to keep clean. My parents’ house, including their bedroom, was carpeted with a beautiful sea green carpet. We were pretty certain that the carpeting would not survive Dad’s home care. One of Stan’s assignments was to figure out how to save the carpet. He eventually decided on chair mats. He bought out the supply of rectangular mats at Staples and Office Max and then worked out the arrangement of the mats in the bedroom. In addition to protecting the floor, the mats provided a relatively hard surface and protected the carpet from some of the heavy equipment and the wheelchair that would be brought into the room. He also purchased some shelving and boxes that we would need for storing medical supplies. Thank goodness my parents’ bedroom was large enough to accommodate everything.
If you spend any time at a hospital, you quickly learn that healthcare is a dirty business and the floor is difficult to keep clean. My parents’ house, including their bedroom, was carpeted with a beautiful sea green carpet. We were pretty certain that the carpeting would not survive Dad’s home care. One of Stan’s assignments was to figure out how to save the carpet. He eventually decided on chair mats. He bought out the supply of rectangular mats at Staples and Office Max and then worked out the arrangement of the mats in the bedroom. In addition to protecting the floor, the mats provided a relatively hard surface and protected the carpet from some of the heavy equipment and the wheelchair that would be brought into the room. He also purchased some shelving and boxes that we would need for storing medical supplies. Thank goodness my parents’ bedroom was large enough to accommodate everything. Shortly after we arrived, I went to the nurses’ station to see Jennifer. She said that she had been waiting for me to arrive so that I could administer Dad’s morning meds. At practically the same time, Dr. Smith arrived and we discussed Dad’s feeding tube and his invasive lines. I agreed with the doctor that because of its upkeep and the potential for infection, we wanted the
Shortly after we arrived, I went to the nurses’ station to see Jennifer. She said that she had been waiting for me to arrive so that I could administer Dad’s morning meds. At practically the same time, Dr. Smith arrived and we discussed Dad’s feeding tube and his invasive lines. I agreed with the doctor that because of its upkeep and the potential for infection, we wanted the  I returned to the hospital at 2:00 P.M. to find that Jennifer and the aide were giving Dad a bath. When they were finished, Jennifer and I maneuvered Dad into the wheelchair. Jennifer thought that he was a bit weaker than yesterday and said that she wanted him back in bed in about an hour. It was a nice day, so after I had Dad cough up some secretions, we headed outside in the wheelchair. We strolled on all of the available sidewalks, which still wasn’t much of an outing, and then settled under the covered hospital entrance. While we were sitting out front, Stan and Mom drove up and visited. Stan could stay for only a couple of minutes because they had been grocery shopping and he had to get the perishables home. Mom and I visited outside with Dad until 3:25 P.M. Shortly after the three of us returned to Dad’s room, Jennifer, Hector, and I put him back in bed. Mom and I visited with Dad until about 4:30 P.M.
I returned to the hospital at 2:00 P.M. to find that Jennifer and the aide were giving Dad a bath. When they were finished, Jennifer and I maneuvered Dad into the wheelchair. Jennifer thought that he was a bit weaker than yesterday and said that she wanted him back in bed in about an hour. It was a nice day, so after I had Dad cough up some secretions, we headed outside in the wheelchair. We strolled on all of the available sidewalks, which still wasn’t much of an outing, and then settled under the covered hospital entrance. While we were sitting out front, Stan and Mom drove up and visited. Stan could stay for only a couple of minutes because they had been grocery shopping and he had to get the perishables home. Mom and I visited outside with Dad until 3:25 P.M. Shortly after the three of us returned to Dad’s room, Jennifer, Hector, and I put him back in bed. Mom and I visited with Dad until about 4:30 P.M. Stan and I stayed up late to watch the total lunar eclipse (blood moon). While watching the moon, my dear friend Rhoda texted me to see how I was doing. I quickly called her to let her know about the miracle and our change in plans.
Stan and I stayed up late to watch the total lunar eclipse (blood moon). While watching the moon, my dear friend Rhoda texted me to see how I was doing. I quickly called her to let her know about the miracle and our change in plans.
 I practically ran back to Dad’s room to tell Mom the good news. Marty stopped by a few minutes later at 2:00 P.M. and asked if we wanted to review some brochures for Home Care providers. We knew that Adan worked for Scott & White Home Care and worked with the physical and occupational therapists that would care for Dad. Ironically, our decision to go with
I practically ran back to Dad’s room to tell Mom the good news. Marty stopped by a few minutes later at 2:00 P.M. and asked if we wanted to review some brochures for Home Care providers. We knew that Adan worked for Scott & White Home Care and worked with the physical and occupational therapists that would care for Dad. Ironically, our decision to go with  Dad was a little tired after dialysis and didn’t feel up to much physical therapy. He didn’t get out of bed but did agree to some exercises in bed. Shortly after Jennifer left Dad’s room, Mom started feeling very lightheaded and faint. I got her a glass of water and I had Dana, the nurse, check her pulse. It was 82, which was fine, but Mom’s lightheadedness didn’t go away. While I watched this unbelievable mini-drama play out, I noticed Dad’s razor sharp focus on Mom that never wavered. I felt like an intruder on an intimate moment. I then asked Dana to take Mom’s blood pressure. Her blood pressure was very high, and the nurses strongly suggested that I take her to the emergency room at Memorial. I couldn’t believe it, and myriad emotions washed over me. Just minutes earlier we had been so elated about Dad, and now I was very worried about my mother. What was it with my parents and their dueling maladies? The nurse fetched a wheelchair while I pulled the car to the front entrance and we drove five miles to Memorial.
Dad was a little tired after dialysis and didn’t feel up to much physical therapy. He didn’t get out of bed but did agree to some exercises in bed. Shortly after Jennifer left Dad’s room, Mom started feeling very lightheaded and faint. I got her a glass of water and I had Dana, the nurse, check her pulse. It was 82, which was fine, but Mom’s lightheadedness didn’t go away. While I watched this unbelievable mini-drama play out, I noticed Dad’s razor sharp focus on Mom that never wavered. I felt like an intruder on an intimate moment. I then asked Dana to take Mom’s blood pressure. Her blood pressure was very high, and the nurses strongly suggested that I take her to the emergency room at Memorial. I couldn’t believe it, and myriad emotions washed over me. Just minutes earlier we had been so elated about Dad, and now I was very worried about my mother. What was it with my parents and their dueling maladies? The nurse fetched a wheelchair while I pulled the car to the front entrance and we drove five miles to Memorial.
 When I arrived, I met Dr. Ciceri and he explained to me that Dad had something that sounded like “the Canada fungus.” He said that they planned to replace his dialysis catheter and his PIC line. The doctor had also started Dad on an antifungal. He said that he requested a TTE (transthoracic echocardiogram) for later today. I didn’t understand the significance of most of what he said, but I clearly understood what he said next. He said that Dad’s prognosis was extremely poor, that he probably had one to two months to live, and would most likely die in a nursing home.
When I arrived, I met Dr. Ciceri and he explained to me that Dad had something that sounded like “the Canada fungus.” He said that they planned to replace his dialysis catheter and his PIC line. The doctor had also started Dad on an antifungal. He said that he requested a TTE (transthoracic echocardiogram) for later today. I didn’t understand the significance of most of what he said, but I clearly understood what he said next. He said that Dad’s prognosis was extremely poor, that he probably had one to two months to live, and would most likely die in a nursing home. At 9:40 P.M., I was awakened by the house phone, and I ran to answer it before it woke Mom. As far as we were concerned, there was nothing worse than a nighttime phone call. My parents’ phone system had an audio caller ID. My heart practically stopped when I heard it announce that the call was from Scott & White. The call was from Jeliza, Dad’s nurse. According to her, Dad insisted that he wanted to go home and that he had seen Mom in the hall. He kept calling out for her, and the nurse couldn’t calm him. She hoped that my mother or I might be more successful. Jeliza held up the phone to Dad’s ear while I explained to him that we had been in his room until 6:00 P.M., but that he had been asleep. He asked me when we would return to see him again, and when I said, “tomorrow,” he asked if we’d come by early. When I told him that we’d see him after dialysis, he said that he wasn’t going to dialysis anymore and that he would go someplace else. I explained that going someplace else would require advance planning and that we couldn’t make alternative plans on a Sunday night. I promised him that Mom and I would be there and that I’d visit with him before I left for Houston. He agreed to that plan and we said good night. The nurse took back the phone and thanked me for talking with him.
At 9:40 P.M., I was awakened by the house phone, and I ran to answer it before it woke Mom. As far as we were concerned, there was nothing worse than a nighttime phone call. My parents’ phone system had an audio caller ID. My heart practically stopped when I heard it announce that the call was from Scott & White. The call was from Jeliza, Dad’s nurse. According to her, Dad insisted that he wanted to go home and that he had seen Mom in the hall. He kept calling out for her, and the nurse couldn’t calm him. She hoped that my mother or I might be more successful. Jeliza held up the phone to Dad’s ear while I explained to him that we had been in his room until 6:00 P.M., but that he had been asleep. He asked me when we would return to see him again, and when I said, “tomorrow,” he asked if we’d come by early. When I told him that we’d see him after dialysis, he said that he wasn’t going to dialysis anymore and that he would go someplace else. I explained that going someplace else would require advance planning and that we couldn’t make alternative plans on a Sunday night. I promised him that Mom and I would be there and that I’d visit with him before I left for Houston. He agreed to that plan and we said good night. The nurse took back the phone and thanked me for talking with him. I left the CCH at 11:40 A.M. to have lunch at the house with Mom and Stan. They had stayed at the house to do some yard work. Mom had found a couple of snake skins, which I took to use with some of my lumen printing. I thought that they might add a nice touch to my fig leaf prints.
I left the CCH at 11:40 A.M. to have lunch at the house with Mom and Stan. They had stayed at the house to do some yard work. Mom had found a couple of snake skins, which I took to use with some of my lumen printing. I thought that they might add a nice touch to my fig leaf prints. Mom and I arrived at Dad’s room around 9:15 A.M. Dad was getting an IV for a heart flutter. I asked the doctor about his restraints and about his plan for removing them. Because the
Mom and I arrived at Dad’s room around 9:15 A.M. Dad was getting an IV for a heart flutter. I asked the doctor about his restraints and about his plan for removing them. Because the  When we were ready to return to the air conditioning, I tried the back door buzzer, which notified the nurses’ station that someone was at the receiving entrance. The nurses kindly told me that it wasn’t safe to go out that door. I took Dad out for one more spin, but through the front door. When we returned to his room, he said that he wanted to go back to his room. I told him that he was in his room. To orient him to his surroundings, I backed him out of his room and pushed him back in. I also showed him his sunflowers and told him that as long as he saw those flowers, he was in his room. He then fell fast asleep. We called Michelle, his nurse, to tell her that we were leaving. She fastened a gait belt around him so that he wouldn’t slide out of the chair and said that they would move him back to bed before the shift change. Mom and I then left at 4:30. We stopped off at HEB and picked up a pizza for our dinner.
When we were ready to return to the air conditioning, I tried the back door buzzer, which notified the nurses’ station that someone was at the receiving entrance. The nurses kindly told me that it wasn’t safe to go out that door. I took Dad out for one more spin, but through the front door. When we returned to his room, he said that he wanted to go back to his room. I told him that he was in his room. To orient him to his surroundings, I backed him out of his room and pushed him back in. I also showed him his sunflowers and told him that as long as he saw those flowers, he was in his room. He then fell fast asleep. We called Michelle, his nurse, to tell her that we were leaving. She fastened a gait belt around him so that he wouldn’t slide out of the chair and said that they would move him back to bed before the shift change. Mom and I then left at 4:30. We stopped off at HEB and picked up a pizza for our dinner.
 Addison, one of the
Addison, one of the  When the three of us arrived at the house, Mom told us that last night she had washed her slippers and had left them on the bench in the courtyard.When she woke up today, only one slipper remained. The neighbors share stories of the wildlife in the area. I decided to try my luck slipper hunting in the backyard. Sure enough, I found it under a tree, none the worse for wear. Something that seemed like a tasty treat must have left its predator with a little dry mouth. Dad would love this story.
When the three of us arrived at the house, Mom told us that last night she had washed her slippers and had left them on the bench in the courtyard.When she woke up today, only one slipper remained. The neighbors share stories of the wildlife in the area. I decided to try my luck slipper hunting in the backyard. Sure enough, I found it under a tree, none the worse for wear. Something that seemed like a tasty treat must have left its predator with a little dry mouth. Dad would love this story.
 When Mom and I arrived at the CCH at 7:45 A.M., Dad was sleeping. A few minutes later, the respiratory therapist woke him, finished his breathing treatment, and administered his oral care. While she was finishing her session with Dad,
When Mom and I arrived at the CCH at 7:45 A.M., Dad was sleeping. A few minutes later, the respiratory therapist woke him, finished his breathing treatment, and administered his oral care. While she was finishing her session with Dad,  At 2:55 P.M., Holly stopped by for a bedside swallow assessment. She came armed with ice, grape juice, and pudding, but Dad totally refused to participate. I couldn’t take it for another minute. After trying unsuccessfully to get him to exert any effort, I yelled at him and left the building. By 3:05 P.M. I was in my car and on my way home. Between the numerous obstacles and his inability to overcome them, I was frustrated to the breaking point and I felt like I was about to explode. I stopped by the house to pick up my computer and drove home–fuming all the way. Once again, it seemed like Dad’s biggest obstacle was Dad.
At 2:55 P.M., Holly stopped by for a bedside swallow assessment. She came armed with ice, grape juice, and pudding, but Dad totally refused to participate. I couldn’t take it for another minute. After trying unsuccessfully to get him to exert any effort, I yelled at him and left the building. By 3:05 P.M. I was in my car and on my way home. Between the numerous obstacles and his inability to overcome them, I was frustrated to the breaking point and I felt like I was about to explode. I stopped by the house to pick up my computer and drove home–fuming all the way. Once again, it seemed like Dad’s biggest obstacle was Dad.