November 30, 2015. I woke up at 3:30 A.M., and Dad and Gale woke about two hours later. Dad’s strength had returned to his pre-CDiff levels, and he was in great spirits. Today he would be assessed for an additional 60 days of home care under Medicare. He had been scheduled for this assessment last week but it was canceled when we were temporarily discharged from home care.
 The parade of provider assessments started with Kathleen, the physical therapist, at 10:30 A.M. She was followed at 11:30 A.M. by Janet, the occupational therapist, and at 1:30 P.M. by Stephanie, the nurse. During Kathleen’s visit, she asked how Dad was being transported to dialysis. We told her that we had wanted to use the HOP, but were still using the Scott & White wheel chair service. On October 26, we had hand-delivered our application in hopes that we could expedite the process. We were told at that time that the approval process might take as long as three weeks. We had now waited more than a month. Being able to use the HOP’s paratransit service would save us $114 per week, and we were anxious to take advantage of the cost savings. We had tried calling, but could not get through to a human. Kathleen was familiar with the HOP organization and immediately used a seemingly secret number to phone the office to check on Dad’s status. During her call, she learned that Dad had been approved on November 10, more than two weeks ago, but somehow his paperwork was misplaced and not mailed to us. We could either wait to have them mail it to us or we could stop by the office later today to pick up the paperwork.
The parade of provider assessments started with Kathleen, the physical therapist, at 10:30 A.M. She was followed at 11:30 A.M. by Janet, the occupational therapist, and at 1:30 P.M. by Stephanie, the nurse. During Kathleen’s visit, she asked how Dad was being transported to dialysis. We told her that we had wanted to use the HOP, but were still using the Scott & White wheel chair service. On October 26, we had hand-delivered our application in hopes that we could expedite the process. We were told at that time that the approval process might take as long as three weeks. We had now waited more than a month. Being able to use the HOP’s paratransit service would save us $114 per week, and we were anxious to take advantage of the cost savings. We had tried calling, but could not get through to a human. Kathleen was familiar with the HOP organization and immediately used a seemingly secret number to phone the office to check on Dad’s status. During her call, she learned that Dad had been approved on November 10, more than two weeks ago, but somehow his paperwork was misplaced and not mailed to us. We could either wait to have them mail it to us or we could stop by the office later today to pick up the paperwork.
During my lunch break, Mom and I drove to the HOP office to retrieve Dad’s ID card and a booklet of regulations. We were told that we would have to call the dispatch office to schedule Dad’s pickup times. When we returned home, Mom called the HOP dispatch office, and I happily called the Scott & White EMS wheelchair van service and canceled Dad’s pickups. Transitioning to the public transit system seemed like a huge milestone.
Shortly after Mom and I returned home from the HOP office, our dear friend Mike called to tell us that he would be passing through Temple en route to Houston from Wisconsin. I had not seen Mike since May 15, 2015, the night that Mom had her stroke. Mike is married to Rhoda, who had come to Houston to help me the day after Mom had her stroke. My parents and I looked forward to seeing him again.
At 2:00 P.M., Kristen arrived for her regularly-scheduled swallow therapy session with Dad. At the end of Dad’s session, she said that Dad was “amazing” and that she wanted me to schedule an appointment for a “cookie swallow” test, otherwise known as a modified barium swallow study (MBSS). She also said that next week Dad would advance from ice chips to applesauce. I was excited, yet scared to death. For so long we had made no progress, and some doctors said that he’d never swallow again. Now, after just a couple of weeks with a speech pathologist, he was about to make a remarkable advancement. On the other hand, after just a couple of weeks working with a speech pathologist, he was going to swallow something that could potentially set him back six months. To say the least, my emotions were all over the map. It didn’t help matters any that my father seemed to have a cavalier attitude about what was happening. He seemed to worry more about tomorrow’s bus ride than he did about protecting his airway.
Kristen left at 4:00 P.M., and after a day of visitors and therapy, Dad was ready for a nap. An hour later, he was awake and ready for happy hour and ice chips. By 6:30 P.M., happy hour and dinner were over, and we were ready for a cutthroat game of cards. Gale was on a roll and won again, although not as handily as she had the previous night.
Our bedtime routine started at 7:30 P.M., and Dad was in bed and ready for trach care by 8:00 P.M. Today, it felt like we were finally back in the groove and back on the road to recovery.
December 1. Dad did not sleep well. He was worried about today’s bus ride to dialysis. At 3:15 A.M., he was the first one awake and was eager to get up. At 3:30 A.M., he asked Gale for the booklet of rules and regulations. He had read that booklet so many times that I was certain that he had it memorized. I’d bet money that he had read the guidelines and rules more than any other HOP rider, and he’d been in possession of it for less than 24 hours.
When I came downstairs at 3:45 A.M., I was a little surprised to see him up. I was even more surprised when I returned from the kitchen 40 minutes later with a cup of coffee and saw that he was dressed and ready to go to dialysis. Needless to say, the very tired Gale was not ready. At 5:00 A.M., the parade of surprises continued when the phone rang. The dispatcher from the HOP called to let us know that the bus was en route to our house and would arrive in a few minutes. When Mom had scheduled his pickup time, she gave them the time that the bus needed to arrive at our house, which was 6:15 A.M. The scheduler interpreted that time as the time that Dad needed to arrive at the dialysis center. After we resolved that misunderstanding, the dispatcher said that the bus would arrive at 6:00 A.M. At 5:50 A.M., they arrived and pulled into my parents’ circular driveway. Mom and I watched as the wheelchair lift was lowered. The driver then wheeled Dad into the bus and ensured that the wheelchair was restrained. After Gale entered the bus, Dad paid his fare of $2, and they were off.
While Dad and Gale were at dialysis, Mom made a cake for Gale. Today was her birthday, and we wanted to celebrate it with her. Our friend Mike arrived a few minutes after 11:00 A.M. I had hoped that Dad would arrive home shortly after his session ended, but the bus did not arrive home until 12:30 P.M. Although Mike needed to be on his way to Houston, he stayed until 1:00 P.M. so that he could visit with Dad.
 Shortly after Mike left, Dad was ready for a nap, and he slept until it was time for him to swallow some ice chips. As he wheeled himself from his room, he stopped by the office to let me know that I should stop for the day because it was time for happy hour.
Shortly after Mike left, Dad was ready for a nap, and he slept until it was time for him to swallow some ice chips. As he wheeled himself from his room, he stopped by the office to let me know that I should stop for the day because it was time for happy hour.
After dinner, we presented Gale with her cake, sang to her, and gave her some cheesy gifts. Had she won at cards, her day would have been perfect, but it was not to be. Tonight was my night to win.
By 8:00 P.M., Dad was in bed and I had administered his meds and trach care. Now that he had had one successful day of public transportation under his belt, I hoped that he would sleep well.
December 2. We all had a good night’s sleep. I slept through my alarm and didn’t wake up until 4:30 A.M., and Dad slept until 6:00 A.M., although he wasn’t ready to leap out of bed even then. He was still in bed when I took a break at 7:00 A.M. to administer his meds and trach care. Dad pointed to his various tubes said that he’d be glad when he could get rid of “all of these wires.” I told him that he was in control of when the tubes would be removed. After he rolled his eyes at me, I reiterated the importance of his physical, occupational, and swallow therapy exercises, which he hated doing. After whistling in the wind for a few minutes, I returned to work and let Gale help him to get ready for the day.
An hour or so later, I heard Gale helping him with his swallowing exercises. He and Mom then ran through the exercises that Janet, the occupational therapist, had left for him.
Michell arrived at 11:20 A.M. and met with Gale so that she could catch up on the events of the past week and learn about the bus service. I think that Michell was relieved to hear that the week had been boring in comparison to her drama-week with us. After Gale left, I gave Michell a hug and told her how grateful we were that she had decided to return.
 Gale had barely pulled out of the driveway when Brenda arrived for Dad’s physical therapy session. Brenda put him through his paces, having him walk 68 feet, march in place, stand on one foot, and stand on his toes. Dad was exhausted when she left and was ready for a nap. However, instead of sleeping until he woke up himself, he instructed Michell to wake him by 2:00 P.M.
Gale had barely pulled out of the driveway when Brenda arrived for Dad’s physical therapy session. Brenda put him through his paces, having him walk 68 feet, march in place, stand on one foot, and stand on his toes. Dad was exhausted when she left and was ready for a nap. However, instead of sleeping until he woke up himself, he instructed Michell to wake him by 2:00 P.M.
A couple of hours after waking from his nap, Dad wanted Michell to help him with some of his exercises. I didn’t know if I had inspired him to exercise or if he was more interested in exercise because he was feeling better. The reason didn’t matter to me, as long as he exercised.
After happy hour and dinner, we played cards. Michell was tonight’s winner. By 8:00 P.M., Dad was in bed and practically asleep.
December 3. Dad was up at his regular time for a dialysis day and was ready when the HOP paratransit bus arrived at 5:40 A.M., which meant that Dad would be at dialysis almost an hour before his scheduled chair time. Ideally, he would be home an hour earlier, too.
I worked for about six hours and then packed up my laptop and drove back to Houston. Tonight was the last night of the semester for my photography class. I had missed most of the semester, and I wanted to attend the final critique. Not only did this class represent some remnant of normalcy for me, I wanted to share some of the holiday biscotti that I had baked.
Dad was finished with dialysis at 10:30 A.M. and was on the bus by 11:00 A.M., but because he was the last stop, he and Michell didn’t arrive home until almost 1:00 P.M. By 1:45 P.M., he was ready for a nap. While I was in Houston, Michell would assume responsibility for the trach care and meds. As has been the case with Gale, I had laid out all of the instructions and refilled the pill dispenser. I would be gone for less than 24 hours, so Michell and I both felt that she would get along fine without me.
During happy hour, Michell prepared more ice chips for Dad. After dinner, the three of them played Oh Hell, and Michell won again. After administering the meds and trach care, Michell had Dad ready for bed by 8:00 P.M. and he was asleep before she was ready for bed.
Unfortunately, Dad didn’t stay asleep very long, and by 11:50 P.M. he was fast awake. When Michell asked him why, he told her that he was thinking about problems. Fortunately for both of them, he drifted back to sleep within 30 minutes.


 Kristin,
Kristin, 
 When Michell and Dad were picked up by the EMS wheelchair van service, Stan and I drove to the dialysis center. I had been very upset that they had removed 2,500 ml from Dad on Thursday, and I intended to express my concern to the charge nurse. For each 1,000 ml removed, a dialysis patient loses 1 kg. After I had explained Dad’s situation, she said that they would just clean his blood today and not remove any fluid from him.
When Michell and Dad were picked up by the EMS wheelchair van service, Stan and I drove to the dialysis center. I had been very upset that they had removed 2,500 ml from Dad on Thursday, and I intended to express my concern to the charge nurse. For each 1,000 ml removed, a dialysis patient loses 1 kg. After I had explained Dad’s situation, she said that they would just clean his blood today and not remove any fluid from him. After I saw Dad weighed, Stan and I left Dad and Michell at the dialysis center so that we could run several errands before Dad returned home. Everything worked in our favor, and we were home by 10:30 A.M. As it turned out, Stan and I didn’t have to rush. Dad and Michell had to wait for the van and didn’t return home until after noon.
After I saw Dad weighed, Stan and I left Dad and Michell at the dialysis center so that we could run several errands before Dad returned home. Everything worked in our favor, and we were home by 10:30 A.M. As it turned out, Stan and I didn’t have to rush. Dad and Michell had to wait for the van and didn’t return home until after noon. Shortly before 2:00 P.M., Dad took a long nap on the couch while we were in the living room because he didn’t want to be away from us. I think that he thought that sleeping on the couch would ensure that he didn’t miss happy hour, but he slept through it. Dozing on the couch might not seem like a big deal, but it was another first for him in his post-hospital life. We had to rely on the oxygen tank and trach bib because we couldn’t bring the oxygen concentrator and nebulizer to the living room, but he was able to receive Nepro during his nap. He slept for about four hours, and we woke him when we finished dinner.
Shortly before 2:00 P.M., Dad took a long nap on the couch while we were in the living room because he didn’t want to be away from us. I think that he thought that sleeping on the couch would ensure that he didn’t miss happy hour, but he slept through it. Dozing on the couch might not seem like a big deal, but it was another first for him in his post-hospital life. We had to rely on the oxygen tank and trach bib because we couldn’t bring the oxygen concentrator and nebulizer to the living room, but he was able to receive Nepro during his nap. He slept for about four hours, and we woke him when we finished dinner. At 10:30 P.M., the baby monitor station in our room started alarming. After quickly putting on my glasses, I could read the message on the display that indicated that our station was unlinked from the base station. As I tried to turn on the light, I discovered that the
At 10:30 P.M., the baby monitor station in our room started alarming. After quickly putting on my glasses, I could read the message on the display that indicated that our station was unlinked from the base station. As I tried to turn on the light, I discovered that the  By 8:00 A.M., Dad was back in the wheelchair and was reading the Sunday newspaper. When Mom and I left for church, he and Stan were playing cribbage. After a couple of games of cribbage, Dad wanted to lie down and rest. According to Michell, he fell asleep as soon as his head hit the pillow. Usually, he liked for us to wake him before Stan left for Houston, but today he asked that we let him sleep.
By 8:00 A.M., Dad was back in the wheelchair and was reading the Sunday newspaper. When Mom and I left for church, he and Stan were playing cribbage. After a couple of games of cribbage, Dad wanted to lie down and rest. According to Michell, he fell asleep as soon as his head hit the pillow. Usually, he liked for us to wake him before Stan left for Houston, but today he asked that we let him sleep. November 23. Dad was very slow in waking up this morning. When I heard him and Michell talking, I took a break from work to administer his morning meds and trach care. Tracy, one of our RNs, called around 9:00 A.M.to see if we could be her first stop this morning. I was very low on the Mepilex dressings that American HomePatient didn’t provide and asked Tracy if she could bring me a few to tide me over until I could order more from Amazon. She said that she would stop by the office and pick up a couple for me. I was very fond of Tracy. She was a wonderful nurse and the mother of a special needs child. She was one of my favorite nurses and a very caring person. She arrived at my parents’ home at 10:00 A.M. with my requested dressing in hand. After her brief examination of Dad, she said that his bed sore was practically healed. With the way that Dad had been feeling, I didn’t want to take him back to the wound care doctor, which would most likely take the entire afternoon. She said that I could safely cancel his appointment with wound care today. Also, she didn’t think that I would need any more of the expensive Mepilex dressings. I happily accepted the good news and canceled the appointment with the doctor and the EMS wheelchair van service.
November 23. Dad was very slow in waking up this morning. When I heard him and Michell talking, I took a break from work to administer his morning meds and trach care. Tracy, one of our RNs, called around 9:00 A.M.to see if we could be her first stop this morning. I was very low on the Mepilex dressings that American HomePatient didn’t provide and asked Tracy if she could bring me a few to tide me over until I could order more from Amazon. She said that she would stop by the office and pick up a couple for me. I was very fond of Tracy. She was a wonderful nurse and the mother of a special needs child. She was one of my favorite nurses and a very caring person. She arrived at my parents’ home at 10:00 A.M. with my requested dressing in hand. After her brief examination of Dad, she said that his bed sore was practically healed. With the way that Dad had been feeling, I didn’t want to take him back to the wound care doctor, which would most likely take the entire afternoon. She said that I could safely cancel his appointment with wound care today. Also, she didn’t think that I would need any more of the expensive Mepilex dressings. I happily accepted the good news and canceled the appointment with the doctor and the EMS wheelchair van service. While Tracy was visiting, Dad spent the entire time either sitting or lying on the bed, so she didn’t see how weak he had become. Shortly before Tracy arrived, Michell had had to hold up Dad to keep him from falling when he was trying to get dressed. I hoped that we would hear something soon from Dr. Pfanner’s office.
While Tracy was visiting, Dad spent the entire time either sitting or lying on the bed, so she didn’t see how weak he had become. Shortly before Tracy arrived, Michell had had to hold up Dad to keep him from falling when he was trying to get dressed. I hoped that we would hear something soon from Dr. Pfanner’s office.
 As Mom and I were driving to church, I told her that I had read the log book that the aides kept about Dad, so I knew about Dad’s fall yesterday. I was pretty irritated that she had decided to withhold this information from me. I was very invested in his care and recovery, and it disturbed me that my parents would choose to keep this information from me. She agreed that they would not withhold this type of information from me again and said that she would talk with Dad after lunch. However, we both hoped that there would be no next time.
As Mom and I were driving to church, I told her that I had read the log book that the aides kept about Dad, so I knew about Dad’s fall yesterday. I was pretty irritated that she had decided to withhold this information from me. I was very invested in his care and recovery, and it disturbed me that my parents would choose to keep this information from me. She agreed that they would not withhold this type of information from me again and said that she would talk with Dad after lunch. However, we both hoped that there would be no next time. While we were at church, Dad told Gale that he was tired and that he wanted to lie down. He also complained about some tightness and soreness in his back. Gale thought that he also seemed a little depressed about yesterday’s fall in the bedroom. The home-patient hospital beds had only two side rails, which did nothing to keep Dad in bed. At one point, I had used pipe cleaners to attach a couple dozen little bells to four chairs that we pushed up against the sides of Dad’s bed. He still might have been able to escape from the bed, but we hoped that the bells would wake at least one of us during an attempted escape. The chairs and bells had worked for about a week but were less effective as Dad got stronger. One side of the bed was partially obstructed because of the oxygen concentrator and nebulizer. While Dad napped, Gale moved the wheelchair to the other side of the bed and locked it in place, which made that bad boy practically impossible to move.
While we were at church, Dad told Gale that he was tired and that he wanted to lie down. He also complained about some tightness and soreness in his back. Gale thought that he also seemed a little depressed about yesterday’s fall in the bedroom. The home-patient hospital beds had only two side rails, which did nothing to keep Dad in bed. At one point, I had used pipe cleaners to attach a couple dozen little bells to four chairs that we pushed up against the sides of Dad’s bed. He still might have been able to escape from the bed, but we hoped that the bells would wake at least one of us during an attempted escape. The chairs and bells had worked for about a week but were less effective as Dad got stronger. One side of the bed was partially obstructed because of the oxygen concentrator and nebulizer. While Dad napped, Gale moved the wheelchair to the other side of the bed and locked it in place, which made that bad boy practically impossible to move. After lunch, Dad read the newspaper in his room and rested until the nurse arrived at 4:20 P.M. She said that Dad’s vitals were great and said that he didn’t have a fever. When she learned about the fall (During every visit, providers ask if you’ve had any falls.) and the difficulty that Gale and Mom had had getting him up off of the floor, she said that we could always call for a nurse for assistance. Regarding the reasons why we had called for a nurse, she could only speculate about the cause of his diarrhea and back pain.
After lunch, Dad read the newspaper in his room and rested until the nurse arrived at 4:20 P.M. She said that Dad’s vitals were great and said that he didn’t have a fever. When she learned about the fall (During every visit, providers ask if you’ve had any falls.) and the difficulty that Gale and Mom had had getting him up off of the floor, she said that we could always call for a nurse for assistance. Regarding the reasons why we had called for a nurse, she could only speculate about the cause of his diarrhea and back pain. Shortly after noon, Tracy, the nurse, stopped by for Dad’s routine Monday checkup. Similar to yesterday, Dad’s vitals were good. I asked her if we could give Dad some Imodium, but she said that she could not give advice about medications. I finally asked her what she would do if she was in my position, and she said that she’d give her father half of a pill.
Shortly after noon, Tracy, the nurse, stopped by for Dad’s routine Monday checkup. Similar to yesterday, Dad’s vitals were good. I asked her if we could give Dad some Imodium, but she said that she could not give advice about medications. I finally asked her what she would do if she was in my position, and she said that she’d give her father half of a pill. After dinner, Dad felt like playing cards, which was our litmus test for how well he was feeling. By 7:30 P.M., I had won, and we were moving Dad toward his bedroom to start the nighttime routine.
After dinner, Dad felt like playing cards, which was our litmus test for how well he was feeling. By 7:30 P.M., I had won, and we were moving Dad toward his bedroom to start the nighttime routine. Fortunately, they didn’t have to wait too long after dialysis for a ride, and Dad and Gale were home by 12:15 P.M. He was pretty wiped out and wanted to take a nap. By 12:40 P.M., he was back on the bed, hooked up to the tube feed and moist air. I administered his trach care and a portion of his midday meds. I became distracted by some shiny object and forgot to administer his antibiotic. Less than five minutes after I left his room, he was sleeping. While he slept, I called Sue, our friend and nurse practitioner at the dialysis center, to see what else I could do for Dad. She said that I could safely give him two pills, the recommended dosage of Imodium.
Fortunately, they didn’t have to wait too long after dialysis for a ride, and Dad and Gale were home by 12:15 P.M. He was pretty wiped out and wanted to take a nap. By 12:40 P.M., he was back on the bed, hooked up to the tube feed and moist air. I administered his trach care and a portion of his midday meds. I became distracted by some shiny object and forgot to administer his antibiotic. Less than five minutes after I left his room, he was sleeping. While he slept, I called Sue, our friend and nurse practitioner at the dialysis center, to see what else I could do for Dad. She said that I could safely give him two pills, the recommended dosage of Imodium. While Gale and I were in Dad’s room running through his nighttime routine, Gale found a little scorpion on the floor near her bed. Gale was one of the most fearless women I knew, but she screamed like a little girl when she saw the critter. We had barely disposed of it when she encountered another one crawling on the bathroom floor toward the bedroom carpet. My parents had found scorpions in the house in the past, but I don’t recall ever seeing one, and tonight we saw two.
While Gale and I were in Dad’s room running through his nighttime routine, Gale found a little scorpion on the floor near her bed. Gale was one of the most fearless women I knew, but she screamed like a little girl when she saw the critter. We had barely disposed of it when she encountered another one crawling on the bathroom floor toward the bedroom carpet. My parents had found scorpions in the house in the past, but I don’t recall ever seeing one, and tonight we saw two.

 November 11. Dad had another good night. I might have heard him cough twice. At 7:45 A.M., I was between meetings and wanted to administer trach care and meds, but Dad was still in bed and didn’t want to get up. I told him that he was a lazy bones and that we’d have to make “
November 11. Dad had another good night. I might have heard him cough twice. At 7:45 A.M., I was between meetings and wanted to administer trach care and meds, but Dad was still in bed and didn’t want to get up. I told him that he was a lazy bones and that we’d have to make “ Before Stephanie’s car left the driveway, Brenda pulled up behind her for Dad’s physical therapy session. I didn’t watch the session, but from what I could hear, it seemed like she was working with him on transfers. I once heard her say that Dad got an A on something that he did, but not an A+. At the end of the session, she said that he got a gold star for the day. I had to laugh to myself as I wondered about the type of psychology that they employed to get him to cooperate. On her way out, Brenda stopped by my office and asked me about the rubber mat for the shower that I had agreed to get during our discussion on
Before Stephanie’s car left the driveway, Brenda pulled up behind her for Dad’s physical therapy session. I didn’t watch the session, but from what I could hear, it seemed like she was working with him on transfers. I once heard her say that Dad got an A on something that he did, but not an A+. At the end of the session, she said that he got a gold star for the day. I had to laugh to myself as I wondered about the type of psychology that they employed to get him to cooperate. On her way out, Brenda stopped by my office and asked me about the rubber mat for the shower that I had agreed to get during our discussion on  November 12. Shortly before 3:30 A.M., I heard Dad call for Gale to help him to find the urinal. I got up shortly after that and woke them. I watched as Gale handled all of the meds and routine trach care this morning—her last practice run before I left for Houston. Everything ran smoothly, and we were ready when the wheelchair van arrived at 5:50 A.M., some 20 minutes early.
November 12. Shortly before 3:30 A.M., I heard Dad call for Gale to help him to find the urinal. I got up shortly after that and woke them. I watched as Gale handled all of the meds and routine trach care this morning—her last practice run before I left for Houston. Everything ran smoothly, and we were ready when the wheelchair van arrived at 5:50 A.M., some 20 minutes early. Gale had her first solo run with the meds and trach care right after I left. Dad took a nap until 3:00 P.M. and was up for the remainder of the day. The three of them played cards, and Mom won again. Gale got Dad in bed by 8:00 P.M. and had no problem administering his night time meds and trach care.
Gale had her first solo run with the meds and trach care right after I left. Dad took a nap until 3:00 P.M. and was up for the remainder of the day. The three of them played cards, and Mom won again. Gale got Dad in bed by 8:00 P.M. and had no problem administering his night time meds and trach care. Stephanie, the nurse, came by around noon to take Dad’s vitals and check his bedsore. She said that the bedsore was healing nicely and that it was looking great. Bless her heart; Stephanie also brought us enough trach lubricant to last for a couple of months. These home care nurses were wonderful. In hindsight, I don’t know if I ever told them how much I appreciated them.
Stephanie, the nurse, came by around noon to take Dad’s vitals and check his bedsore. She said that the bedsore was healing nicely and that it was looking great. Bless her heart; Stephanie also brought us enough trach lubricant to last for a couple of months. These home care nurses were wonderful. In hindsight, I don’t know if I ever told them how much I appreciated them.
 Today started out pretty well for Dad—in fact, it seemed practically transformative. He was able to pull himself up in the bed with one hand, and his transfers from the bed to the wheelchair were much better. When Tracy, the nurse, stopped by at 10:00 A.M., she said that he was doing well and that his bed sore seemed to be healing. Janet, the occupational therapist, arrived about 90 minutes later and put him through the paces with some arm and core exercises. On her way out, she said that she thought that Dad was progressing very well.
Today started out pretty well for Dad—in fact, it seemed practically transformative. He was able to pull himself up in the bed with one hand, and his transfers from the bed to the wheelchair were much better. When Tracy, the nurse, stopped by at 10:00 A.M., she said that he was doing well and that his bed sore seemed to be healing. Janet, the occupational therapist, arrived about 90 minutes later and put him through the paces with some arm and core exercises. On her way out, she said that she thought that Dad was progressing very well. Last Sunday I had purchased a couple of pumpkins from the church. Tomorrow was Halloween, which was Gale’s favorite holiday. She usually spent the day with her granddaughters and was a little disappointed that she was missing this time with them. I had searched the internet for her to find some
Last Sunday I had purchased a couple of pumpkins from the church. Tomorrow was Halloween, which was Gale’s favorite holiday. She usually spent the day with her granddaughters and was a little disappointed that she was missing this time with them. I had searched the internet for her to find some  The storm passed through the area pretty fast, and it wasn’t raining at 6:15 A.M. when Dad and Gale were picked up for dialysis by the EMTs. Because it was Saturday, Mom and I ate breakfast together and tried to catch up on some chores around the house. While our lives were revolving around Dad, our household was like a computer. Mom acted as the operating system that managed our primary functions, like shopping, laundry, cleaning, and meal preparation. I kept up with Dad’s appointments, meds, supplies, and trach care. The aides handled Dad’s most basic needs and monitored his safety, and Stan helped with the yard and filled in all of the gaps. He also provided the extra dose of testosterone in the house, which Dad needed.
The storm passed through the area pretty fast, and it wasn’t raining at 6:15 A.M. when Dad and Gale were picked up for dialysis by the EMTs. Because it was Saturday, Mom and I ate breakfast together and tried to catch up on some chores around the house. While our lives were revolving around Dad, our household was like a computer. Mom acted as the operating system that managed our primary functions, like shopping, laundry, cleaning, and meal preparation. I kept up with Dad’s appointments, meds, supplies, and trach care. The aides handled Dad’s most basic needs and monitored his safety, and Stan helped with the yard and filled in all of the gaps. He also provided the extra dose of testosterone in the house, which Dad needed. Mom and I searched the house for the pills, but we couldn’t find them anywhere. We surmised that we must have inadvertently thrown out that prescription when we threw away the bag from the pharmacy. This was our first major system failure since Dad had come home. Mom and I opted to forget about the antifungal—for now. It was less than 45 days ago that we were told that Dad would die from a fungus in his blood. I didn’t like the idea of forgoing this medication. Tomorrow was Sunday and I would see Sue, the dialysis nurse practitioner, at church. I hoped that she might have some suggestions on what we should do. Meanwhile, we felt as if the tricking had started already, and not the treating.
Mom and I searched the house for the pills, but we couldn’t find them anywhere. We surmised that we must have inadvertently thrown out that prescription when we threw away the bag from the pharmacy. This was our first major system failure since Dad had come home. Mom and I opted to forget about the antifungal—for now. It was less than 45 days ago that we were told that Dad would die from a fungus in his blood. I didn’t like the idea of forgoing this medication. Tomorrow was Sunday and I would see Sue, the dialysis nurse practitioner, at church. I hoped that she might have some suggestions on what we should do. Meanwhile, we felt as if the tricking had started already, and not the treating. After our happy hour and a spaghetti dinner, I decided that we wanted a group Halloween photo, and I herded everyone outside to the front porch.
After our happy hour and a spaghetti dinner, I decided that we wanted a group Halloween photo, and I herded everyone outside to the front porch. I needed to get back to Houston periodically for a day or two. I had contacted a couple of services to see if we could hire nurses to handle Dad’s trach care, but we needed someone three times a day, and I couldn’t figure out how to make it work logistically or financially. I also learned that it wasn’t every nurse that was trained to handle the duties of a respiratory therapist. I had approached Gale a couple of days earlier to see if she would be willing to administer the meds and trach care for Dad while I was gone. I planned to have everything set up and documented for her. Administering the medication was pretty simple with our pill organizer and pill crusher. The trach care was a trickier issue. I was pleased when she said that she would try administering the trach care a couple of times to see if she could handle it.
I needed to get back to Houston periodically for a day or two. I had contacted a couple of services to see if we could hire nurses to handle Dad’s trach care, but we needed someone three times a day, and I couldn’t figure out how to make it work logistically or financially. I also learned that it wasn’t every nurse that was trained to handle the duties of a respiratory therapist. I had approached Gale a couple of days earlier to see if she would be willing to administer the meds and trach care for Dad while I was gone. I planned to have everything set up and documented for her. Administering the medication was pretty simple with our pill organizer and pill crusher. The trach care was a trickier issue. I was pleased when she said that she would try administering the trach care a couple of times to see if she could handle it.
 commode that we kept in the common area of the bathroom. Having it in a more open area enabled the aides to transport him to and from the commode, a contraption that he loathed. After helping him into the bathroom to use the dreaded bedside commode, Gale and I were able to convince him to go back to bed. Thankfully, he remained in bed until 8:30 A.M., at which time I administered his trach care and morning meds. I was still a rookie with the trach care and the process took about 45 minutes.
commode that we kept in the common area of the bathroom. Having it in a more open area enabled the aides to transport him to and from the commode, a contraption that he loathed. After helping him into the bathroom to use the dreaded bedside commode, Gale and I were able to convince him to go back to bed. Thankfully, he remained in bed until 8:30 A.M., at which time I administered his trach care and morning meds. I was still a rookie with the trach care and the process took about 45 minutes. also needed to bring a blanket, a box of tissues, and various other items. Gale told Stan that instead of Mom’s Elizabeth Arden tote bag that we were using to transport his dialysis accessories, Dad needed something larger and more masculine, like a duffle bag. Stan wasn’t sure what she had in mind, but he eventually found a gym bag that she deemed perfect for the task.
also needed to bring a blanket, a box of tissues, and various other items. Gale told Stan that instead of Mom’s Elizabeth Arden tote bag that we were using to transport his dialysis accessories, Dad needed something larger and more masculine, like a duffle bag. Stan wasn’t sure what she had in mind, but he eventually found a gym bag that she deemed perfect for the task. During dialysis, Dad used oxygen tanks from the dialysis center, but this service did not include the moisture that he needed to keep his trach moist. In an attempt to compensate for the lack of moisture, Timothy from American HomePatient had provided us with several bibs composed of a porous non-woven material. The bib was placed between the trach and the oxygen source. The bib wouldn’t stay moist for more than 30 minutes, so we kept a small spray bottle in his dialysis bag, and Gale was vigilant about keeping the bib wet.
During dialysis, Dad used oxygen tanks from the dialysis center, but this service did not include the moisture that he needed to keep his trach moist. In an attempt to compensate for the lack of moisture, Timothy from American HomePatient had provided us with several bibs composed of a porous non-woven material. The bib was placed between the trach and the oxygen source. The bib wouldn’t stay moist for more than 30 minutes, so we kept a small spray bottle in his dialysis bag, and Gale was vigilant about keeping the bib wet.
 September 12. Mom and I arrived at the CCH at 8:00 A.M. Dad was still restrained and his call button was on the floor. John, Dad’s nurse, told us that his heart rate had been elevated to 135 and he became
September 12. Mom and I arrived at the CCH at 8:00 A.M. Dad was still restrained and his call button was on the floor. John, Dad’s nurse, told us that his heart rate had been elevated to 135 and he became 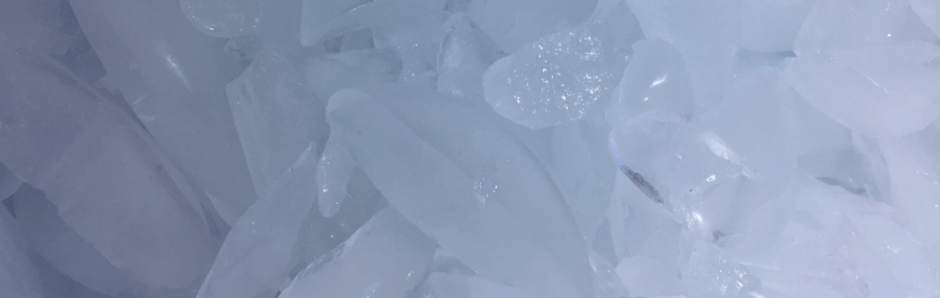
 Addison, one of the
Addison, one of the  When the three of us arrived at the house, Mom told us that last night she had washed her slippers and had left them on the bench in the courtyard.When she woke up today, only one slipper remained. The neighbors share stories of the wildlife in the area. I decided to try my luck slipper hunting in the backyard. Sure enough, I found it under a tree, none the worse for wear. Something that seemed like a tasty treat must have left its predator with a little dry mouth. Dad would love this story.
When the three of us arrived at the house, Mom told us that last night she had washed her slippers and had left them on the bench in the courtyard.When she woke up today, only one slipper remained. The neighbors share stories of the wildlife in the area. I decided to try my luck slipper hunting in the backyard. Sure enough, I found it under a tree, none the worse for wear. Something that seemed like a tasty treat must have left its predator with a little dry mouth. Dad would love this story.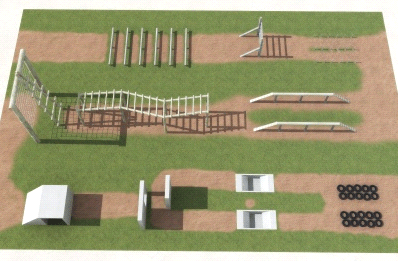
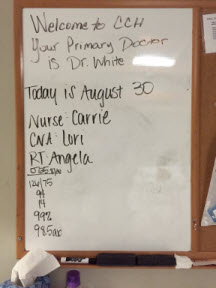 When Mom and I arrived at the CCH at 7:45 A.M., Dad was sleeping. A few minutes later, the respiratory therapist woke him, finished his breathing treatment, and administered his oral care. While she was finishing her session with Dad,
When Mom and I arrived at the CCH at 7:45 A.M., Dad was sleeping. A few minutes later, the respiratory therapist woke him, finished his breathing treatment, and administered his oral care. While she was finishing her session with Dad,  At 2:55 P.M., Holly stopped by for a bedside swallow assessment. She came armed with ice, grape juice, and pudding, but Dad totally refused to participate. I couldn’t take it for another minute. After trying unsuccessfully to get him to exert any effort, I yelled at him and left the building. By 3:05 P.M. I was in my car and on my way home. Between the numerous obstacles and his inability to overcome them, I was frustrated to the breaking point and I felt like I was about to explode. I stopped by the house to pick up my computer and drove home–fuming all the way. Once again, it seemed like Dad’s biggest obstacle was Dad.
At 2:55 P.M., Holly stopped by for a bedside swallow assessment. She came armed with ice, grape juice, and pudding, but Dad totally refused to participate. I couldn’t take it for another minute. After trying unsuccessfully to get him to exert any effort, I yelled at him and left the building. By 3:05 P.M. I was in my car and on my way home. Between the numerous obstacles and his inability to overcome them, I was frustrated to the breaking point and I felt like I was about to explode. I stopped by the house to pick up my computer and drove home–fuming all the way. Once again, it seemed like Dad’s biggest obstacle was Dad.