September 5, 2015. When we opened the Temple Daily Telegram, we were greeted with the unfortunate news of another Scott & White doctor dying, this time in a climbing accident. Scott & White had now lost two doctors during Dad’s hospitalization.
I arrived at Dad’s room at 9:45 A.M. The window shades were open, but the lights were off and he was still asleep. The first thing that I noticed was that he was restrained with his wrists bound to the side rails, which prevented him from being able to call for assistance or suction himself. I used the call button to call the nurse, but she cut me off while I was speaking. I was pretty annoyed when I called her, but being cut off mid-sentence really irked me. I stormed out of Dad’s room to the nurses’ station and told the nurse that if she was going to leave him in a helpless state, I expected her to stop by his room every 15 minutes to tend him, or loosen the restraints to the point that he could suction himself. The nurse and respiratory therapist accompanied me back into Dad’s room. The three of us were followed by the charge nurse, who gave me a dressing down for yelling at her nurses at the nurses’ station. I wasn’t yelling, but there was no doubt that I sounded very annoyed. As I walked back to Dad’s room, I asked them if they possessed any humanity at all.
As Dad woke up, he started becoming agitated about his restraints. He also kept saying that he was done here and wanted to leave. Who could blame him?
At 10:20 A.M., Alyssa, his nurse, stopped by to tend to a wound on his right foot. She also tended to his oral care for the morning. Dad wasn’t wild about having his teeth cleaned, but he finally let her do it. I tried my best to explain how important oral care was to his situation, but he didn’t believe that we were helping him.
At 10:40 A.M., a couple of nurses stopped by to reposition him. I had to remind them to give him enough slack in his restraints so that he could suction himself.
 I left the CCH at 11:40 A.M. to have lunch at the house with Mom and Stan. They had stayed at the house to do some yard work. Mom had found a couple of snake skins, which I took to use with some of my lumen printing. I thought that they might add a nice touch to my fig leaf prints.
I left the CCH at 11:40 A.M. to have lunch at the house with Mom and Stan. They had stayed at the house to do some yard work. Mom had found a couple of snake skins, which I took to use with some of my lumen printing. I thought that they might add a nice touch to my fig leaf prints.
Mom and I returned to the hospital at 2:00 P.M. Dad kept wanting to get out of bed, and I kept trying to get him to understand that he had to follow the rules and stay in bed or else they would restrain him. Alyssa then told me that Dr. Anderson wanted Dad restrained 24/7.
At 2:45 P.M., his feeding tube became clogged. Alyssa couldn’t clear it, so she went to enlist some help from Melissa, another nurse. While she was out of the room, Victor, the respiratory therapist, came in to clean Dad’s trach dressing and to suction him. Dad had mentioned to me that he didn’t like this respiratory therapist. He would insert the suction tube down the trach to the point that Dad would gag, then he’d sort of giggle and push it deeper until Dad’s legs would shake. It was a disturbing spectacle to watch and wasn’t typical of all of the respiratory therapists.
While he was in the room, Victor told us that Dad was still be being suctioned a few times a day. Until Dad could remove his secretions better, they couldn’t contemplate red-capping him.
After Victor left, I gave Dad a bunch of pep talks about coughing and suctioning to the point that he asked me if I was his cheerleader. Sometimes I could be a little over the top, but I felt like I was practically willing him to improve.
At 4:10 P.M., the nurses came back to Dad’s room to try to clear out his clogged feeding tube. They tried moving him around in the bed to see if the movement would help clear up the clog. They then loosened up the tie on his right hand so that he could use it to hold the Yankauer, his suctioning wand. After they had given him some slack in the restraints he said that he usually used his left hand for the Yankauer, which made the nurses laugh. They changed the restraints again so that he could suction himself with his left hand.
Mom and I left for home around 4:30 P.M. Dad looked so lonely. I hated to leave him. On the way out, one of the nurses told us that he had asked her for scissors. When she told him that she couldn’t do that, he told her that she wouldn’t have to tell anyone about it. Everything about Dad’s behavior seemed so surreal. He was delirious to the point that he was like a different person, but occasionally his sense of humor surfaced. Even the nurse thought his request was funny.
Stan treated Mom and me to a dinner at J&B’s. After dinner, we stopped back by the hospital to say goodnight to Dad, but he was asleep. The only person who saw us was Victor.
I was so worried about Dad and his restraints. I just couldn’t envision the doctor ever having them removed. Of course, it would have been nice to see Dr. Anderson so that we could discuss it. When we did catch sight of him, he just walked by without acknowledging our presence.
Although Dad’s hands were restrained, his feet weren’t. Three times during the night, Connie, his nurse, found him with both of his legs dangling out of the side of the bed. Before putting his legs back in the bed, she tried to convince him that he needed to keep his legs in the bed.
September 6. Before we went to the CCH, I emailed three of my best friends about an upcoming trip to Wisconsin that was scheduled for late September. The trip was a birthday gift from my girlfriends and I was looking forward to the break. My Dad’s condition had been a little touch-and-go recently, but I was still hopefully optimistic that he would be well enough for me to feel comfortable leaving him for five days.
 Mom and I arrived at Dad’s room around 9:15 A.M. Dad was getting an IV for a heart flutter. I asked the doctor about his restraints and about his plan for removing them. Because the Seroquel didn’t seem to be addressing his delirium, the doctor told me that he was switching him to Risperidone. He said that Dad pulled out his feeding tube three times overnight. I believed him at the time, but there was nothing in Dad’s chart that supported such a statement. When I asked about what was keeping him at the CCH, he said that they needed to check to see whether the dialysis center would take him.
Mom and I arrived at Dad’s room around 9:15 A.M. Dad was getting an IV for a heart flutter. I asked the doctor about his restraints and about his plan for removing them. Because the Seroquel didn’t seem to be addressing his delirium, the doctor told me that he was switching him to Risperidone. He said that Dad pulled out his feeding tube three times overnight. I believed him at the time, but there was nothing in Dad’s chart that supported such a statement. When I asked about what was keeping him at the CCH, he said that they needed to check to see whether the dialysis center would take him.
In the last day or so, it seemed that Dad had lost his manual dexterity, which affected his ability to suction himself. It was hard to watch him fumble with the Yankauer and not be able to hold it up to his mouth. Mom and I agreed that we should ask the doctor to see if Dad could have some occupational therapy to help regain his ability to suction himself.
Mom and I left for church shortly after 10:00 A.M. and Stan stayed with Dad during our absence. At church, the sermon was about waiting. Sometimes it seemed like the pastor wrote his sermons specifically for us.
After lunch, Mom and I returned to the hospital around 2:00 P.M. Dad announced that he was ready for a ride in the chair.
Michelle got him in the Stryker chair, showed me how to use it, and we took off. It’s a wild chair with wheels that move independently of each other, so you can move sideways. With Mom in charge of the portable oxygen tank and me in charge of driving the chair, we went up and down the halls, out the front door and back in. I also took him towards the back of the hospital and out the delivery doors, which was where he entered this place via ambulance. The doors opened easily enough to let us out, but they did not reopen when we tried to return. As long as we were outside, I tried to give Dad the lay of the land. When my parents first moved to Temple, they lived just a short distance from this facility. He really had no concept of where he was, and I think that he enjoyed the time outside and the mini geography lesson.
 When we were ready to return to the air conditioning, I tried the back door buzzer, which notified the nurses’ station that someone was at the receiving entrance. The nurses kindly told me that it wasn’t safe to go out that door. I took Dad out for one more spin, but through the front door. When we returned to his room, he said that he wanted to go back to his room. I told him that he was in his room. To orient him to his surroundings, I backed him out of his room and pushed him back in. I also showed him his sunflowers and told him that as long as he saw those flowers, he was in his room. He then fell fast asleep. We called Michelle, his nurse, to tell her that we were leaving. She fastened a gait belt around him so that he wouldn’t slide out of the chair and said that they would move him back to bed before the shift change. Mom and I then left at 4:30. We stopped off at HEB and picked up a pizza for our dinner.
When we were ready to return to the air conditioning, I tried the back door buzzer, which notified the nurses’ station that someone was at the receiving entrance. The nurses kindly told me that it wasn’t safe to go out that door. I took Dad out for one more spin, but through the front door. When we returned to his room, he said that he wanted to go back to his room. I told him that he was in his room. To orient him to his surroundings, I backed him out of his room and pushed him back in. I also showed him his sunflowers and told him that as long as he saw those flowers, he was in his room. He then fell fast asleep. We called Michelle, his nurse, to tell her that we were leaving. She fastened a gait belt around him so that he wouldn’t slide out of the chair and said that they would move him back to bed before the shift change. Mom and I then left at 4:30. We stopped off at HEB and picked up a pizza for our dinner.
Labor Day, September 7. Mom and I arrived at the CCH at 1:00 P.M. Dad usually returned to his room from dialysis between 1:00 P.M. and 1:30 P.M., so we were surprised to see him and Michelle, his nurse, in the room. The lights were off, with the only light coming from the small windows. Michelle was at his bedside with a couple of vials of blood in her hands. She said that he had had a bad morning and that his blood pressure had dropped and his MAP had dipped into the 50s. Because of his low blood pressure, they ended his session an hour early. They removed only 64 ml of fluid, a tiny amount, and had just cleaned his blood during the session. She said that the normal dose of Midodrine that he usually took for his blood pressure didn’t help so they started him on some vasopressors, which finally increased his MAP to 65. The doctor ordered a blood workup to see if Dad was developing a sepsis condition. The nurse said that he was rousable, but he seemed pretty knocked out to us.
Michelle said that he had been more responsive before dialysis, but he was becoming less responsive. When the nurse tried to get a response from him, he scowled in pain, but wouldn’t open his eyes. The nurse said that they would check his venous blood gases and that they also ordered some blood cultures, but they wouldn’t get those results for a couple of days. The doctor came back and said that Dad was like just this before he got sick last time, which didn’t make sense to me because his condition had been improving before he aspirated in July. He added that Dad might be in septic shock again, but he didn’t know why yet. In the meantime, he ordered an additional broad-based antibiotic—in addition to the one that he was already taking.
Stan and I had traveled to Temple in one car and I hadn’t brought my computer with me, so I couldn’t stay in Temple. We had planned to leave at 2:00 P.M., but I asked Stan if we could wait an hour longer. I hated to leave my parents with my father in this condition. I left Dad’s room and called Mom’s friend, Marilyn, to see if she could stop by to stay with Mom for a while. Like a true friend in time of need, she said that she would arrive by 3:00 P.M. When I returned to his room, he started to wake up. He quickly got annoyed with the pneumatic compression devices (PCD) on his legs, and he asked why this keeps happening to him.
The doctor also suspected that Dad had acquired CDiff. Until they received the results of that lab work, they had to assume that he had it. While we were in Dad’s room, the nurse taped an isolation sign on the door. I stayed and visited with him a little longer, and then I told him goodbye, and he kissed me goodbye.
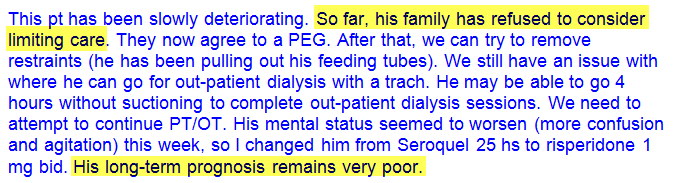
Mom was very concerned that the doctor caused Dad’s worsening problems. While she was probably wrong, we sensed some attitude from this doctor, and found the following note from him in Dad’s chart:
Stan picked me up at the CCH shortly after 3:00 P.M. and I said goodbye to Mom and Marilyn.
Stan and I encountered heavy traffic during our drive back into Houston. It seemed as if everyone was returning to Houston at the same time. When we got to Buc-ee’s, about 40 miles from home, Stan stopped for a beverage. While he was inside, I called Mom to check on Dad. She said that he was doing better and that Michelle had rolled him onto his side, and he fell asleep. What was interesting about this news was that Dad had always slept on his side, and this was probably the first time during his hospitalization that he was rolled onto his side. His myriad devices and restraints had been forcing him to sleep on his back.


 Addison, one of the
Addison, one of the  When the three of us arrived at the house, Mom told us that last night she had washed her slippers and had left them on the bench in the courtyard.When she woke up today, only one slipper remained. The neighbors share stories of the wildlife in the area. I decided to try my luck slipper hunting in the backyard. Sure enough, I found it under a tree, none the worse for wear. Something that seemed like a tasty treat must have left its predator with a little dry mouth. Dad would love this story.
When the three of us arrived at the house, Mom told us that last night she had washed her slippers and had left them on the bench in the courtyard.When she woke up today, only one slipper remained. The neighbors share stories of the wildlife in the area. I decided to try my luck slipper hunting in the backyard. Sure enough, I found it under a tree, none the worse for wear. Something that seemed like a tasty treat must have left its predator with a little dry mouth. Dad would love this story.
 When Mom and I arrived at the CCH at 7:45 A.M., Dad was sleeping. A few minutes later, the respiratory therapist woke him, finished his breathing treatment, and administered his oral care. While she was finishing her session with Dad,
When Mom and I arrived at the CCH at 7:45 A.M., Dad was sleeping. A few minutes later, the respiratory therapist woke him, finished his breathing treatment, and administered his oral care. While she was finishing her session with Dad,  At 2:55 P.M., Holly stopped by for a bedside swallow assessment. She came armed with ice, grape juice, and pudding, but Dad totally refused to participate. I couldn’t take it for another minute. After trying unsuccessfully to get him to exert any effort, I yelled at him and left the building. By 3:05 P.M. I was in my car and on my way home. Between the numerous obstacles and his inability to overcome them, I was frustrated to the breaking point and I felt like I was about to explode. I stopped by the house to pick up my computer and drove home–fuming all the way. Once again, it seemed like Dad’s biggest obstacle was Dad.
At 2:55 P.M., Holly stopped by for a bedside swallow assessment. She came armed with ice, grape juice, and pudding, but Dad totally refused to participate. I couldn’t take it for another minute. After trying unsuccessfully to get him to exert any effort, I yelled at him and left the building. By 3:05 P.M. I was in my car and on my way home. Between the numerous obstacles and his inability to overcome them, I was frustrated to the breaking point and I felt like I was about to explode. I stopped by the house to pick up my computer and drove home–fuming all the way. Once again, it seemed like Dad’s biggest obstacle was Dad. Mom had been encouraged
Mom had been encouraged 
 With the exception of a couple of golf tournaments, Dad hadn’t been watching any television since May 6. To catch him up on the latest political happenings, Mom brought him the Newsweek magazine that had Donald Trump’s picture on the cover. At the time, Mr. Trump still didn’t seem like he’d make it to the general election, let alone the White House.
With the exception of a couple of golf tournaments, Dad hadn’t been watching any television since May 6. To catch him up on the latest political happenings, Mom brought him the Newsweek magazine that had Donald Trump’s picture on the cover. At the time, Mr. Trump still didn’t seem like he’d make it to the general election, let alone the White House. Today was dialysis day, so Mom and I spent the morning at home doing chores and picked 284 tomatoes from the vegetable garden. We had picked so many tomatoes this summer that Mom and I were eating tomato sandwiches every day—sometimes twice a day. We arrived at the CCH at 12:30 P.M. and encountered
Today was dialysis day, so Mom and I spent the morning at home doing chores and picked 284 tomatoes from the vegetable garden. We had picked so many tomatoes this summer that Mom and I were eating tomato sandwiches every day—sometimes twice a day. We arrived at the CCH at 12:30 P.M. and encountered  August 23. Sundays at the CCH were pretty uneventful. There was no dialysis or therapies and you didn’t see the doctors after the morning rounds unless there was a problem. You’d think that the parking lot would be full of cars, but the CCH wasn’t teeming with visitors. The place seemed empty, dark, and depressing. The doctors at Memorial had told me on more than one occasion that a primary reason for transferring Dad from the ICU to the CCH was so that he could be exposed to more light. These rooms had small windows and even with all the light on, the rooms still seemed dark.
August 23. Sundays at the CCH were pretty uneventful. There was no dialysis or therapies and you didn’t see the doctors after the morning rounds unless there was a problem. You’d think that the parking lot would be full of cars, but the CCH wasn’t teeming with visitors. The place seemed empty, dark, and depressing. The doctors at Memorial had told me on more than one occasion that a primary reason for transferring Dad from the ICU to the CCH was so that he could be exposed to more light. These rooms had small windows and even with all the light on, the rooms still seemed dark. Pam said that she spoke with the doctors about Dad’s delirium, and they wanted to fully vent him at night and had ordered an extra dose of
Pam said that she spoke with the doctors about Dad’s delirium, and they wanted to fully vent him at night and had ordered an extra dose of  Five minutes later, the EMTs arrived to prepare Dad for the trip back to CCH. Because the cuff was deflated on his trach collar, Dad was able to chat with the EMTs without a speaking valve. He seemed to be in good spirits and didn’t exhibit any agitated behavior. The EMTs’ preparations were finished in less than 30 minutes. As they started pushing Dad’s gurney out of his room, Dawn rushed into the room with Dad’s
Five minutes later, the EMTs arrived to prepare Dad for the trip back to CCH. Because the cuff was deflated on his trach collar, Dad was able to chat with the EMTs without a speaking valve. He seemed to be in good spirits and didn’t exhibit any agitated behavior. The EMTs’ preparations were finished in less than 30 minutes. As they started pushing Dad’s gurney out of his room, Dawn rushed into the room with Dad’s  Dr. Stewart then told me and Mom that he wanted to meet with us in a conference room to consult with us about some of Dad’s future possibilities. He started off this consultation by stating that they considered Dad’s recovery to be one of their best achievements and acknowledged our part in that success. He went on to say that he suspected that if Dad did go home, he could have more episodes of pneumonia. He continued by saying that Dad might never fully develop the ability to swallow, and if he did, he could very likely choke on his food and develop pneumonia again. He went on to say that although Dad might never be able to eat peas and carrots, we should let him eat what he wants, regardless of the consequences. He said that there was a good chance that Dad would go home with a trach tube. After that disheartening meeting with one of our favorite caregivers, Mom and I returned to Dad’s room.
Dr. Stewart then told me and Mom that he wanted to meet with us in a conference room to consult with us about some of Dad’s future possibilities. He started off this consultation by stating that they considered Dad’s recovery to be one of their best achievements and acknowledged our part in that success. He went on to say that he suspected that if Dad did go home, he could have more episodes of pneumonia. He continued by saying that Dad might never fully develop the ability to swallow, and if he did, he could very likely choke on his food and develop pneumonia again. He went on to say that although Dad might never be able to eat peas and carrots, we should let him eat what he wants, regardless of the consequences. He said that there was a good chance that Dad would go home with a trach tube. After that disheartening meeting with one of our favorite caregivers, Mom and I returned to Dad’s room.


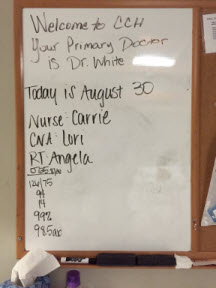
 August 9, 2015. We arrived at the hospital at 9:00 A.M. to find that Dad was still asleep and restrained, the nurse’s name was not on the board, and Dad’s feeding tube was empty. Two out of three of these situations were unacceptable. I went to the nurse’s station to find out who his nurse was and to let them know that his tube feed bottle was empty. A nurse entered the room with a fresh bottle of Nepro, changed out his tubing, and replaced the empty bottle. The nurse also told me that Dad’s nurse was Nicole, who finally showed up at 9:15 A.M. and introduced herself.
August 9, 2015. We arrived at the hospital at 9:00 A.M. to find that Dad was still asleep and restrained, the nurse’s name was not on the board, and Dad’s feeding tube was empty. Two out of three of these situations were unacceptable. I went to the nurse’s station to find out who his nurse was and to let them know that his tube feed bottle was empty. A nurse entered the room with a fresh bottle of Nepro, changed out his tubing, and replaced the empty bottle. The nurse also told me that Dad’s nurse was Nicole, who finally showed up at 9:15 A.M. and introduced herself.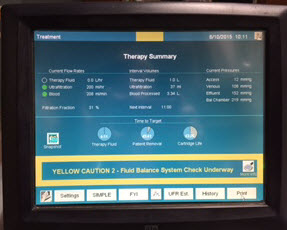 August 10. We arrived at 7:40 A.M. and noticed that Dad was already on dialysis. Before we arrived, they had drawn blood and ran an
August 10. We arrived at 7:40 A.M. and noticed that Dad was already on dialysis. Before we arrived, they had drawn blood and ran an 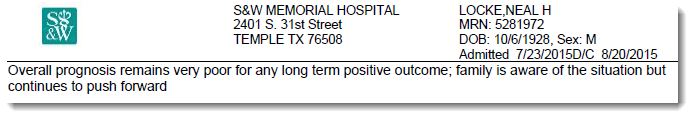

 August 7, 2015. Mom and I arrived at the hospital at 7:45 A.M. Dad was still receiving CPAP breathing support. We were surprised to see that he was not having dialysis, but we had scarcely put down our purses when Lucy, the dialysis nurse, stopped by and said that she had been told to set up the (traditional) four-hour dialysis session. As she left the room,
August 7, 2015. Mom and I arrived at the hospital at 7:45 A.M. Dad was still receiving CPAP breathing support. We were surprised to see that he was not having dialysis, but we had scarcely put down our purses when Lucy, the dialysis nurse, stopped by and said that she had been told to set up the (traditional) four-hour dialysis session. As she left the room,  August 8. Mom and I arrived at Dad’s room at 6:30 A.M. The room was dark and Dad was still sleeping. Jennifer, his nurse, arrived at 7:30 A.M. and started her morning assessment of Dad. When she was finished, she told us that the night nurse told her that Dad was very agitated during the night. I wasn’t sure what that meant, but it didn’t sound good. On a more positive note, Dad’s WBC count was still trending downward.
August 8. Mom and I arrived at Dad’s room at 6:30 A.M. The room was dark and Dad was still sleeping. Jennifer, his nurse, arrived at 7:30 A.M. and started her morning assessment of Dad. When she was finished, she told us that the night nurse told her that Dad was very agitated during the night. I wasn’t sure what that meant, but it didn’t sound good. On a more positive note, Dad’s WBC count was still trending downward.