August 25, 2015. Dad had a good night, and by “good,” I mean that he stayed in bed and didn’t try to pull out any vital devices. Dr. White thought that Dad was pleasant and could answer most of his assessment questions, but Dad’s cognition waxed and waned, depending on the time of day. The doctor said that until Dad regained some of his strength, he wasn’t going to consider red-capping the trach, let alone removing it.
The healthcare providers weren’t the only ones who thought that Dad was confused about his whereabouts. Dad thought that he was at home and Mom had to explain to him that he was at the hospital and home was where she went at the end of every day.
Another of Dad’s problems was severe protein calorie malnutrition. I felt partly to blame because I had practically insisted that they reduce his tube feeds during dialysis. I couldn’t help how I felt. There was no way that Dad could survive another aspiration event.
 Mom had been encouraged yesterday when Dad seemed interested in signing the paperwork necessary to obtain matching funds from Shell for the Locke Academic Scholarship at CMU. Unfortunately, although he was still very interested in the scholarship, he couldn’t sign his name. Mom gave him a pen, but he didn’t seem interested in practicing, either. She thought that perhaps she could sign the form for him if they could get a notary to witness his intent and consent. Mom told the CCH chaplain of their predicament and he said that a notary public worked at the CCH. He said that he would see what he could do for them.
Mom had been encouraged yesterday when Dad seemed interested in signing the paperwork necessary to obtain matching funds from Shell for the Locke Academic Scholarship at CMU. Unfortunately, although he was still very interested in the scholarship, he couldn’t sign his name. Mom gave him a pen, but he didn’t seem interested in practicing, either. She thought that perhaps she could sign the form for him if they could get a notary to witness his intent and consent. Mom told the CCH chaplain of their predicament and he said that a notary public worked at the CCH. He said that he would see what he could do for them.
When she was notified about Mom’s request, Marty, from the administration office, stopped by Dad’s room and told Mom that because of Dad’s mentation problems and confusion, the CCH’s notary could not witness any signatures on his behalf. She went on to say that because finances were involved, the notary at the CCH could not notarize the patient’s document. Sometimes Marty annoyed the heck out of me. Instead of simply stating that the CCH was not permitted to notarize financial documents, she made a point of stating that Dad was not of sound mind. The bottom line was that he could have been as sharp as a tack, and they wouldn’t have been able to help my parents. I could not understand why so often the staff at this facility felt the need to go above and beyond to demoralize patients and their families.
At 1:30 P.M., Jennifer, the physical therapy assistant, stopped by for Dad’s therapy. Dad told her that other than a pain in his right shoulder, he was feeling pretty good today. He also kept mentioning to her that he had a document that he needed to get notarized. Jennifer had her work cut out for her to keep Dad focused on his exercises, but she was able to get him to finish some bed exercises and to sit on the edge of the bed. She had to use her hand to keep Dad from falling over on the bed. She wasn’t able to get him to stand up, but after he finished his physical therapy session, Jennifer and Carrie, the nurse, put Dad in a cardiac chair that they referred to as the Stryker chair. This chair was totally cool and much different from the cardiac chairs at Memorial. It had four wheels that turned independently of each other. When you pushed him in this chair, you had the flexibility of moving sideways and in circles. Unfortunately, you could also move in those directions when you were trying to move in a straight line. Today he simply sat in the chair in his room.
A couple of hours after Mom went home, and at the time of the shift change, the bed alarm sounded in Dad’s room. The night nurse, Debra, hurried into Dad’s room and found him on the floor. Evidently, he had decided that he could get out of the bed to use the bathroom. As soon as he stood up, he pretty much sat down on the floor. With the assistance of another nurse, Debra got him back into bed and reset the bed alarm to its most sensitive setting.
Less than three hours later Dad’s bed alarm sounded again. This time, Debra reached Dad’s room before he got out of bed. She reminded him again that he needed to use the call button when he needed assistance. Before leaving the room, she raised three of the side rails on his bed. Because Dad often scooted down the bed and sort of slid out of the bed through the open rail, I asked if it could also be raised. I was informed by the nurses that raising all four rails was synonymous with restraining a patient, at least in the eyes of Texas law.
Dad was able to stay in bed for the remainder of the evening.
August 26. Today marked another ominous milestone. It was the 90th day since Dad started dialysis, which officially made him ESRD (end-stage renal disease), or dialysis dependent. The 90th day was also dialysis day and Rebecca, his nurse, darkened his door at 7:00 A.M. and wheeled him up to the dialysis center for another eight-hour session.
When Mom arrived at the hospital at 11:30 A.M., she learned that Dad’s WBC count was down to 6.5, which was very normal. Dad’s room was empty, so she asked when the patients usually returned from dialysis. Rebecca said that he would be finished sometime between 1:00-1:30 P.M. Instead of waiting for a couple of hours in his room, Mom decided to drive over to Memorial to speak with the Scott & White SeniorCare Insurance representative. Dad was fast approaching what we were told was the end of his hospitalization insurance coverage and Mom needed to learn more about where he stood and what sort of options were available to us.
Shortly after Mom returned to the hospital she learned about Dad’s escape and attempted escape from the bed last night.
After Dad returned to his room, he asked Mom about his brothers and how many boys his middle brother, Jim, had. He also told Mom that he had been taken away to some special place. Mom explained to him that he had been having dreams and that he hadn’t been taken anywhere, except for dialysis, which was located in the CCH. After Mom clarified the confusion about Dad’s nephews, they seemed to have a more coherent conversation.
 With the exception of a couple of golf tournaments, Dad hadn’t been watching any television since May 6. To catch him up on the latest political happenings, Mom brought him the Newsweek magazine that had Donald Trump’s picture on the cover. At the time, Mr. Trump still didn’t seem like he’d make it to the general election, let alone the White House.
With the exception of a couple of golf tournaments, Dad hadn’t been watching any television since May 6. To catch him up on the latest political happenings, Mom brought him the Newsweek magazine that had Donald Trump’s picture on the cover. At the time, Mr. Trump still didn’t seem like he’d make it to the general election, let alone the White House.
Before Mom left for the day, Pastor Don stopped by for a visit. He always seemed to instinctively know when to stop by and cheer up my parents, and he provided the perfect end to Mom’s day at the hospital.
August 27. The blood test results that I used to live by now seemed to be hanging out in the normal zone. You’d think that I would have started to exhale, but I was still very worried about the infection that seemed to lurk in his lungs. It didn’t help matters much that Dr. White had requested another consult from infectious diseases. We hadn’t seen Dr. Sangeetha Ranganath for a few weeks. Mom didn’t catch everything that the doctor said, but Mom did hear that she changed Dad’s antibiotic.
A few days earlier, Dad had had me write down 16 exercises that he planned to perform to build up his strength. Before I returned home to Houston, he had instructed me to leave the list of exercises in his room where he could find them. He seemed months away from being able to perform any of the exercises, but when Jennifer stopped by today for his physical therapy session, he was fixated on them. He kept telling Jennifer that he wanted her to find the exercises for him to complete. She finally was able to redirect him to the task at hand and got him to perform some of the bed exercises, but he flat out refused to perform sit-stands or sit in the chair; in fact, he insisted on getting back into bed. She and Mom both tried to explain how these exercises were important for building his strength, but their pleas fell on deaf ears. Who knows; maybe he wasn’t wearing his hearing aids. Mom was very discouraged. She and I were desperate for Dad to build up his strength, yet he seemed unwilling to participate.
The hospitals were starting to take a toll on Mom. During the past month, she had developed a cough that she couldn’t seem to shake. The danged place was always cold, and she and I kept sweaters in Dad’s room. Throughout the day, she popped cough drops to soothe her throat.
August 28. I drove to Temple this morning and arrived at my parents’ house while my father was still on dialysis. Mom and I met briefly with Dr. Heath White before Dad returned to his room. The doctor said that he had met with Dad earlier and he seemed to be feeling pretty well today. As usual, he mentioned Dad’s waxing and waning delirium, but he also mentioned that his WBC count was holding steady at 6.5. Dad was a little late returning to his room because he had been scheduled for a chest CT scan immediately after dialysis.
The doctor recommended that they replace Dad’s nasal feeding tube with a PEG, which is inserted into the stomach through the abdominal wall, rather than the nose. My father-in-law had had a terrible experience with the PEG, which heavily influenced me to avoid it. I also was concerned with my father’s penchant for pulling out vital invasive devices. Pulling out a nasal tube is one thing; pulling out a PEG would be something far more serious. We told Dr. White that we would consider his recommendation. He was now the third doctor who had recommended this procedure. I surely wish that we had gone the PEG route during his initial stay in Memorial. Perhaps he wouldn’t have aspirated if he had had a PEG. We’d never know, but I had my suspicions.
Dad seemed to be in good spirits when he returned to his room. I hadn’t seen him for several days, and he seemed glad to see me again. We spent a few minutes catching up on the past week, but our conversation deteriorated into a discussion about him leaving. No matter what Mom and I said, he couldn’t understand why he couldn’t go home today.
I decided to leave the room for a few minutes and stopped by the business office to talk with someone about Dad’s remaining benefits. I knew that Mom had spoken with them while I was in Houston, but I was still confused about where we stood and what our options were. Marty was available and she explained that Dad had 35 more days of hospital coverage. She also explained that we would be able to get 100 days of coverage from a skilled nursing facility (SNiF). Other than the fact that I knew that one of my cousins had been in a SNiF, I didn’t know much about them.
Shortly after I returned to the room, Jennifer stopped by for a physical therapy session with Dad. He greeted her by telling her that he felt that he could stand and sit in the chair in his room, versus the cardiac chair. However, she hadn’t been in his room very long before he started complaining of fatigue, which was common for dialysis days. He also told her that he wanted to go home today. Although patients usually get into the Stryker chair from a lying-down position, Jennifer said that she would show Dad how he could stand and pivot into the chair from the bed. Dad felt that he was up to the task and was surprised when he couldn’t do it. Jennifer tried to use his failure to complete the task as a teaching moment about the importance of physical therapy, but I didn’t think that it did much good. She was able to transfer him to the chair after she put a gait belt on him.
Dad stayed in the chair for the remainder of the afternoon. Considering how dialysis usually saps his strength, he was having a pretty good afternoon. While he was still in the chair, the respiratory therapist stopped by and said that his breathing had improved and that they probably would not need to put him back on CPAP tonight.
Around 4:00 P.M., I called for Michelle, his nurse, to help move him back into bed. Dad had had a full day and was starting to get tired. Except for the few tense minutes of discussion about leaving, we had had a pretty good day. Mom and I left the hospital hoping that Dad would sleep well.

 Pam said that she spoke with the doctors about Dad’s delirium, and they wanted to fully vent him at night and had ordered an extra dose of
Pam said that she spoke with the doctors about Dad’s delirium, and they wanted to fully vent him at night and had ordered an extra dose of  Five minutes later, the EMTs arrived to prepare Dad for the trip back to CCH. Because the cuff was deflated on his trach collar, Dad was able to chat with the EMTs without a speaking valve. He seemed to be in good spirits and didn’t exhibit any agitated behavior. The EMTs’ preparations were finished in less than 30 minutes. As they started pushing Dad’s gurney out of his room, Dawn rushed into the room with Dad’s
Five minutes later, the EMTs arrived to prepare Dad for the trip back to CCH. Because the cuff was deflated on his trach collar, Dad was able to chat with the EMTs without a speaking valve. He seemed to be in good spirits and didn’t exhibit any agitated behavior. The EMTs’ preparations were finished in less than 30 minutes. As they started pushing Dad’s gurney out of his room, Dawn rushed into the room with Dad’s  Dr. Stewart then told me and Mom that he wanted to meet with us in a conference room to consult with us about some of Dad’s future possibilities. He started off this consultation by stating that they considered Dad’s recovery to be one of their best achievements and acknowledged our part in that success. He went on to say that he suspected that if Dad did go home, he could have more episodes of pneumonia. He continued by saying that Dad might never fully develop the ability to swallow, and if he did, he could very likely choke on his food and develop pneumonia again. He went on to say that although Dad might never be able to eat peas and carrots, we should let him eat what he wants, regardless of the consequences. He said that there was a good chance that Dad would go home with a trach tube. After that disheartening meeting with one of our favorite caregivers, Mom and I returned to Dad’s room.
Dr. Stewart then told me and Mom that he wanted to meet with us in a conference room to consult with us about some of Dad’s future possibilities. He started off this consultation by stating that they considered Dad’s recovery to be one of their best achievements and acknowledged our part in that success. He went on to say that he suspected that if Dad did go home, he could have more episodes of pneumonia. He continued by saying that Dad might never fully develop the ability to swallow, and if he did, he could very likely choke on his food and develop pneumonia again. He went on to say that although Dad might never be able to eat peas and carrots, we should let him eat what he wants, regardless of the consequences. He said that there was a good chance that Dad would go home with a trach tube. After that disheartening meeting with one of our favorite caregivers, Mom and I returned to Dad’s room.




 August 7, 2015. Mom and I arrived at the hospital at 7:45 A.M. Dad was still receiving CPAP breathing support. We were surprised to see that he was not having dialysis, but we had scarcely put down our purses when Lucy, the dialysis nurse, stopped by and said that she had been told to set up the (traditional) four-hour dialysis session. As she left the room,
August 7, 2015. Mom and I arrived at the hospital at 7:45 A.M. Dad was still receiving CPAP breathing support. We were surprised to see that he was not having dialysis, but we had scarcely put down our purses when Lucy, the dialysis nurse, stopped by and said that she had been told to set up the (traditional) four-hour dialysis session. As she left the room,  August 8. Mom and I arrived at Dad’s room at 6:30 A.M. The room was dark and Dad was still sleeping. Jennifer, his nurse, arrived at 7:30 A.M. and started her morning assessment of Dad. When she was finished, she told us that the night nurse told her that Dad was very agitated during the night. I wasn’t sure what that meant, but it didn’t sound good. On a more positive note, Dad’s WBC count was still trending downward.
August 8. Mom and I arrived at Dad’s room at 6:30 A.M. The room was dark and Dad was still sleeping. Jennifer, his nurse, arrived at 7:30 A.M. and started her morning assessment of Dad. When she was finished, she told us that the night nurse told her that Dad was very agitated during the night. I wasn’t sure what that meant, but it didn’t sound good. On a more positive note, Dad’s WBC count was still trending downward. August 3, 2015. It had now been 90 days since Dad first entered the hospital for his seven-to-ten day stay. When Mom and I arrived at 7:45 A.M., Dad’s room was a hubbub of activity. Dr. Phan, the nephrology resident, was assessing him and Emily, his nurse, was exercising his arms and legs. But the first thing that we noticed was Dad’s bed. Yesterday, Dr. Jimenez had told Dad’s nurse that he wanted to see Dad’s bed raised to a more upright position. I had envisioned that the angle of his bed would change from 30 to 75 degrees. What we saw instead was a bed that had morphed into a chair. It played music, automatically adjusted to specific angles, and could change into a chair. Was there anything that this bed couldn’t do?
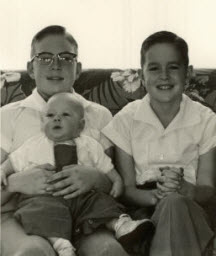
August 3, 2015. It had now been 90 days since Dad first entered the hospital for his seven-to-ten day stay. When Mom and I arrived at 7:45 A.M., Dad’s room was a hubbub of activity. Dr. Phan, the nephrology resident, was assessing him and Emily, his nurse, was exercising his arms and legs. But the first thing that we noticed was Dad’s bed. Yesterday, Dr. Jimenez had told Dad’s nurse that he wanted to see Dad’s bed raised to a more upright position. I had envisioned that the angle of his bed would change from 30 to 75 degrees. What we saw instead was a bed that had morphed into a chair. It played music, automatically adjusted to specific angles, and could change into a chair. Was there anything that this bed couldn’t do? While Mom and I were at home for dinner, I printed out some recent photos of Dad with the family. I wanted the hospital personnel to see him as more than the sick man that they attended in that hospital bed. He hadn’t entered the hospital as some sickly old man, and I wanted them to have a sense of who he was just a few months earlier. After dinner, Mom and I returned to the hospital around 6:50 P.M. and learned that Dustin was Dad’s nurse. I wasn’t impressed with this nurse, and I wasn’t thrilled to see him again.
While Mom and I were at home for dinner, I printed out some recent photos of Dad with the family. I wanted the hospital personnel to see him as more than the sick man that they attended in that hospital bed. He hadn’t entered the hospital as some sickly old man, and I wanted them to have a sense of who he was just a few months earlier. After dinner, Mom and I returned to the hospital around 6:50 P.M. and learned that Dustin was Dad’s nurse. I wasn’t impressed with this nurse, and I wasn’t thrilled to see him again. Shortly after 10:00 A.M., we met
Shortly after 10:00 A.M., we met  When Dad was transferred from the CCH to Memorial, his flowers could not come with him. Cut flowers and plants are not permitted in the ICU. I had been thinking about it for a couple of days, and I was now determined to brighten up Dad’s room. After lunch, I cleaned the vase that had held his sunflower arrangement, took it back to
When Dad was transferred from the CCH to Memorial, his flowers could not come with him. Cut flowers and plants are not permitted in the ICU. I had been thinking about it for a couple of days, and I was now determined to brighten up Dad’s room. After lunch, I cleaned the vase that had held his sunflower arrangement, took it back to  July 28, 2015. Six days since Dad returned to
July 28, 2015. Six days since Dad returned to  The big surprise of the week occurred right after Dr. White left Dad’s room. During the procession of residents and the attending physician, a woman kept appearing in the doorway, and would then leave. When the room was finally empty of providers, she entered Dad’s room and introduced herself as Aimee from the Patient Relations department. She told us that a hospital employee had contacted her office about Dad, and suggested that she meet with us about the events that led to his return to Memorial. I pulled out my iPad of notes and shared our concerns about some of our interactions with one of the CCH doctors. Aimee told us that they would investigate our complaint and get back to us in 30 days. I assured her that although we had complaints about one person, for the most part, we were pleased with the level of care that Dad had received from his providers. When she left, Mom and I were stunned and kept trying to guess who contacted Aimee’s office.
The big surprise of the week occurred right after Dr. White left Dad’s room. During the procession of residents and the attending physician, a woman kept appearing in the doorway, and would then leave. When the room was finally empty of providers, she entered Dad’s room and introduced herself as Aimee from the Patient Relations department. She told us that a hospital employee had contacted her office about Dad, and suggested that she meet with us about the events that led to his return to Memorial. I pulled out my iPad of notes and shared our concerns about some of our interactions with one of the CCH doctors. Aimee told us that they would investigate our complaint and get back to us in 30 days. I assured her that although we had complaints about one person, for the most part, we were pleased with the level of care that Dad had received from his providers. When she left, Mom and I were stunned and kept trying to guess who contacted Aimee’s office. His pulse was running in the 130s again, and his oxygen saturation levels were low. To compensate for the low oxygen levels, the respiratory therapist increased his oxygen levels on the ventilator to 60%. A few minutes later, the ventilator started alarming, which prompted the nurse to page the respiratory therapist. Evidently, one piece of the ventilator was cross-threaded, which was what caused the system to alarm. The alarms were starting to drive us crazy and I could swear that I could hear them when we were away from the hospital.
His pulse was running in the 130s again, and his oxygen saturation levels were low. To compensate for the low oxygen levels, the respiratory therapist increased his oxygen levels on the ventilator to 60%. A few minutes later, the ventilator started alarming, which prompted the nurse to page the respiratory therapist. Evidently, one piece of the ventilator was cross-threaded, which was what caused the system to alarm. The alarms were starting to drive us crazy and I could swear that I could hear them when we were away from the hospital. When Dr. White and his band of providers arrived outside of Dad’s room, I heard comments about Dad being
When Dr. White and his band of providers arrived outside of Dad’s room, I heard comments about Dad being  Shortly before 4:00 P.M., I was presented with a
Shortly before 4:00 P.M., I was presented with a