 August 9, 2015. We arrived at the hospital at 9:00 A.M. to find that Dad was still asleep and restrained, the nurse’s name was not on the board, and Dad’s feeding tube was empty. Two out of three of these situations were unacceptable. I went to the nurse’s station to find out who his nurse was and to let them know that his tube feed bottle was empty. A nurse entered the room with a fresh bottle of Nepro, changed out his tubing, and replaced the empty bottle. The nurse also told me that Dad’s nurse was Nicole, who finally showed up at 9:15 A.M. and introduced herself.
August 9, 2015. We arrived at the hospital at 9:00 A.M. to find that Dad was still asleep and restrained, the nurse’s name was not on the board, and Dad’s feeding tube was empty. Two out of three of these situations were unacceptable. I went to the nurse’s station to find out who his nurse was and to let them know that his tube feed bottle was empty. A nurse entered the room with a fresh bottle of Nepro, changed out his tubing, and replaced the empty bottle. The nurse also told me that Dad’s nurse was Nicole, who finally showed up at 9:15 A.M. and introduced herself.
My annoyance diminished somewhat when Nicole provided me with Dad’s latest lab results. His WBC count was still dropping and had reached 14.9, down from 16.4 yesterday. His liver function was only slightly elevated, which was fantastic news.
Dr. Nidhi Munshi, the weekend nephrologist, stopped by at 9:30 A.M. and told us that Dad would have an eight-hour dialysis session tomorrow.
Stan arrived at 10:00 A.M. and was soon followed by Dr. Vazquez and his entourage. We removed Dad’s restraints and told the nurse that Stan would be there until lunchtime and he would watch Dad to ensure that he didn’t pull out any of his lines and devices. They put him back on CPAP, but said that it seemed that his brain would sometimes forget to breathe when he was asleep. When we met with Stan during lunch, he told us that Dad had been fine and not become agitated while Mom and I were at church.
After lunch, Stan returned to Houston, Mom went back to the hospital, and I stayed home to catch up on some work. When Mom returned home, she said that they received the results from his blood test on Friday and he didn’t seem to have any infections present in his blood. Shortly after she had arrived after lunch, they had changed his ventilator from CPAP to pressure support, which meant that he was breathing on his own. Dad had refused to use his letter board and he couldn’t get a speaking valve until he could breathe on his own, so we were making some progress.
Mom and I returned to the hospital around 7:10 P.M. and were delighted to see that Tyler was Dad’s nurse. He hadn’t been assigned to Dad for several days. Tyler said that he noticed an improvement in Dad. While Mom and I were visiting, Dad seemed to be over-breathing the ventilator. His blood pressure was higher this evening, too. When I mentioned to Tyler that he’d be NPO after midnight because of a TEE scheduled for Monday, Tyler said that he didn’t know about the TEE. Mom and I just looked at each other and rolled our eyes. We headed for home at 8:20 P.M.
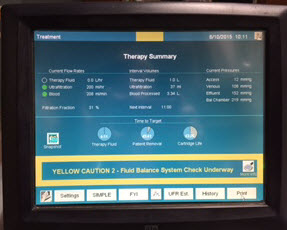 August 10. We arrived at 7:40 A.M. and noticed that Dad was already on dialysis. Before we arrived, they had drawn blood and ran an ABG test and found that his pH was up to 7.53, which meant that, instead of being acidosic, his pH was too alkaline. We were told that they could fix his current pH level by reducing the bicarb dialysate that he received during dialysis.
August 10. We arrived at 7:40 A.M. and noticed that Dad was already on dialysis. Before we arrived, they had drawn blood and ran an ABG test and found that his pH was up to 7.53, which meant that, instead of being acidosic, his pH was too alkaline. We were told that they could fix his current pH level by reducing the bicarb dialysate that he received during dialysis.
Dr. Evan Hardegree stopped by to get the TEE consent forms signed and told us that he’d be assisting Dr. Elizabeth Ebert. It was a coincidence that the cardiologist who was performing the TEE happened to be my parents’ doctor. I still hadn’t gotten used to the fact that once you entered the hospital, you dealt with only the hospital’s doctors and not your own. I hadn’t seen Dr. Ebert since May 19, the first time that Dad had aspirated.
Dr. Lu Pan stopped by to talk with us again about testing Dad on the four-hour dialysis session. He assured us that they would adjust the amount of fluid removed if Dad’s blood pressure dropped too much. Once again, the discussion about these conventional dialysis sessions was increasing my stress level. The back story to the discussion about the shorter dialysis was that they were prepping him for a transfer to the CCH.
Around 9:00 A.M., the cardiology team, led by Dr. Ebert, stopped by with the equipment necessary for the bedside TEE. While they were trying to decide whether the Fentanyl already in Dad’s system would be enough to keep him comfortable during the procedure, Svenja, the trach nurse arrived for a routine follow-up visit. The new tube was supposed to help wean him from the ventilator and she was concerned that Dad had not been on CPAP support much since she replaced the tube.
Mom and I left the room at 9:05 A.M. and passed the time by getting some coffee from the cafeteria. Sometimes the volunteers offered free coffee from their cart, but their coffee was pretty bad. I was no coffee connoisseur, but even I had standards, albeit low. As we arrived in the ICU waiting room, Dr. Hardegree met us and told us that they couldn’t detect any sign of infection on the new arterial valve. Yay!
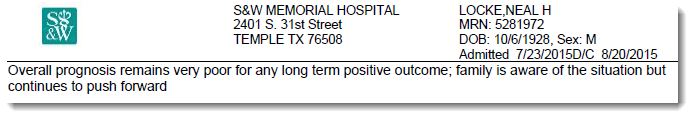
Dr. White came by about 11:00 A.M. and was a real Debbie Downer. I had been feeling a little positive about Dad’s improved condition. In addition to the good news about the TEE, Dad’s WBC count was down to 13.1. When I looked for some positive feedback from the good doctor, he said that although Dad was better than he was when he first arrived, the doctor was not convinced that Dad’s condition would ever improve. Furthermore, because of Dad’s recurring apneic spells, he wasn’t sure that Dad would ever get off the ventilator, and he questioned whether Dad’s mentation would ever improve. When I told him that Dad had just had a TEE and that he was still partially sedated, he was not moved. I felt sick. If Dr. White was right, my father would never forgive us for trapping him in this hellish existence. Dr. White was one of the doctors who had a strong enough voice that Dad might be able to hear what he said, and I was very worried that Dad might have overheard this dismal prognosis. Mom said Dad’s condition seemed to improve after he received physical therapy. Dr. White said that they would try that and that they’d try to find him the cardiac chair.
After lunch, Mom returned to the hospital and I stayed home and tried to accomplish something at work. Sometimes I felt guilty for logging on to work and sending Mom back to the hospital to deal with our alternate existence.
When Mom returned home, she had a mixed report about the afternoon. It seemed to her that Dad had finally bonded with her again. We don’t know why he had been giving her the cold shoulder, but the problem seemed to have resolved itself.

Dad had been in an inside room for several days, and the doctor thought that a window room might help Dad with his mentation and delirium problems. With an inside room, there’s no real sense of day and night. When his nurse was able to round up a couple of other nurses to assist her, she moved Dad to room 238. The hospital was still undergoing a massive facade overhaul, so the window rooms weren’t all that quiet.
After Dad was moved, the nurses were able to move him into a cardiac chair. It’s an amazing contraption that starts as a bed and then morphs into a chair. Dad was still in the chair when PT arrived. The therapist was able to adjust Dad’s position in the chair, but Dad could not sustain an upright sitting position. He just kept slipping down the chair and didn’t seem to have the strength or inclination to sit upright.
Pastor Tom, the senior pastor from their church, stopped by to see Dad. Dad was sleeping, but Tom said that he’d try to visit again tomorrow.
When Mom and I returned to the hospital at 6:55 P.M., we were thrilled to see that Tyler was Dad’s nurse for the night. It had been a stressful day, with more downs than ups. Knowing that Dad was in good hands for the night always helped me and Mom rest better at night. I was still very disturbed about Dr. White’s prognosis and kept replaying the conversation in my head. During my nightly call with Stan, I was pretty upset by the events of the day.
August 11. Mom and I arrived at the hospital at 7:45 A.M. and noticed two things: Dad was restrained and he appeared to have had a bath and shave the previous night. We got Olga, his nurse, to remove the restraints. He immediately started grabbing at his lines and we had a difficult time with him for a while, but he eventually calmed down after they repositioned him. Dr. Hayek stopped by at 8:00 A.M. and adjusted the ventilator for CPAP. He said that Dad had been on CPAP for about 3-5 hours yesterday. I was pleasantly surprised because I thought he had been on CPAP support for only an hour. The other good news for the morning was Dad’s WBC count: it was now down to 12.2.
The fancy schmancy hospital beds were best suited for persons up to 5’10” in height. Dad was 6’1” and often would lie diagonally in the bed. In this diagonal position, he often started slipping out of the bed. We mentioned the problem to Olga, and she was able to find one of the few bed extensions, which added enough length to accommodate Dad’s frame so that he could lie straight in relative comfort without slipping.
Around 10:15 A.M., my parents’ next-door neighbors, LoSharis and Tom, stopped by for a short visit. Dad seemed to brighten up as they entered the room. He immediately recognized Tom and extended his arm to shake hands. I hoped that they would return soon. It seemed as if the fog that surrounded Dad was lifted while they were in the room. Mom had to run some errands, so she left shortly after Tom and LoSharris.
Dr. White made his rounds at 11:00 A.M. When he entered the room, I looked him straight in the eye and told him that Dad was wearing his hearing aids today, and that I’d appreciate it if he would respect that. He paused for a moment, nodded as if he understood the point that I was trying to make, and said, “OK.” Today’s meeting went better than yesterday’s, and Dr. White admitted that Dad appeared to be a lot more alert. I explained to him again that yesterday Dad had just had the TEE when the doctor rounded, so it hadn’t been a fair assessment. To his credit, he agreed that timing was everything.
Nothing positive happens around here without the other shoe dropping, and today was no exception. Dr. White said that he wanted to start Dad on four-hour dialysis trials to prepare him for a transfer to the CCH. I told him that I needed plenty of advance notice because we wanted to meet with April Jones, the CCH nurse manager, before he transferred. We had some concerns about the care that he had received there. Dr. White said that he also would like to hear my concerns and would be available to talk with me anytime. He wanted some specifics about the CCH and I told him about our first 12 nightmarish days there. I also told him that because the place was so dark it didn’t seem like a good environment for someone who was suffering from delirium. From what I could surmise, my comments seemed to fall on deaf ears.
When Dr. White left, I found a quiet place in the hospital to attend an online meeting for work. When I returned from my meeting, Dad was sitting in the cardiac chair. He started getting fidgety and then he experienced some breathing problems. The respiratory therapist was called, and she adjusted his ventilator settings.
After running her errands, Mom returned to the hospital at 1:00 P.M., and I left the hospital a few minutes later so that I could work online from home for a few hours.
Dad sat in the cardiac chair for about another hour. He kept squirming and sliding out of it and was finally moved back into the bed. As soon as he got back into bed, he fell asleep and slept until Mom went home for dinner.
Mom and I returned at 7:10 P.M. and learned that Tyler was taking care of Dad again! We were very surprised because Tyler had already worked three days this week. He told us that he was working five days this week. I was so glad to see him that I forgot that I was opposed to nurses working 60-hour weeks. Seeing him was a relief and felt like the answer to a prayer.

 August 7, 2015. Mom and I arrived at the hospital at 7:45 A.M. Dad was still receiving CPAP breathing support. We were surprised to see that he was not having dialysis, but we had scarcely put down our purses when Lucy, the dialysis nurse, stopped by and said that she had been told to set up the (traditional) four-hour dialysis session. As she left the room,
August 7, 2015. Mom and I arrived at the hospital at 7:45 A.M. Dad was still receiving CPAP breathing support. We were surprised to see that he was not having dialysis, but we had scarcely put down our purses when Lucy, the dialysis nurse, stopped by and said that she had been told to set up the (traditional) four-hour dialysis session. As she left the room,  August 8. Mom and I arrived at Dad’s room at 6:30 A.M. The room was dark and Dad was still sleeping. Jennifer, his nurse, arrived at 7:30 A.M. and started her morning assessment of Dad. When she was finished, she told us that the night nurse told her that Dad was very agitated during the night. I wasn’t sure what that meant, but it didn’t sound good. On a more positive note, Dad’s WBC count was still trending downward.
August 8. Mom and I arrived at Dad’s room at 6:30 A.M. The room was dark and Dad was still sleeping. Jennifer, his nurse, arrived at 7:30 A.M. and started her morning assessment of Dad. When she was finished, she told us that the night nurse told her that Dad was very agitated during the night. I wasn’t sure what that meant, but it didn’t sound good. On a more positive note, Dad’s WBC count was still trending downward. August 5, 2015. When Mom and I arrived this morning, Dr. Brett Ambroson, the resident, was finishing up his morning assessment of Dad’s current status. We were pleased to learn that the vomiting episodes from the previous day had stopped. Dr. Ambroson also noted that Dad would now move his extremities when prompted by him or the other care providers. When I asked about Dad’s WBC count, the doctor said that it was down slightly from yesterday. I wasn’t thrilled with the very slight decrease, but at least the steady upward trend had been arrested. While speaking with Dr. Ambroson, Lucy and Cheryl, the dialysis nurse and her aide, prepared Dad for another eight-hour session.
August 5, 2015. When Mom and I arrived this morning, Dr. Brett Ambroson, the resident, was finishing up his morning assessment of Dad’s current status. We were pleased to learn that the vomiting episodes from the previous day had stopped. Dr. Ambroson also noted that Dad would now move his extremities when prompted by him or the other care providers. When I asked about Dad’s WBC count, the doctor said that it was down slightly from yesterday. I wasn’t thrilled with the very slight decrease, but at least the steady upward trend had been arrested. While speaking with Dr. Ambroson, Lucy and Cheryl, the dialysis nurse and her aide, prepared Dad for another eight-hour session. I returned to the hospital at 6:30 P.M., armed with a couple of small bottles of water. The physical therapist had told me that lifting the bottles while in bed would be good exercise for Dad. Unfortunately, he wouldn’t touch the bottles. I tried talking with him and shared some of his improved lab results with him, but nothing helped. I even tried to make a deal with him and told him that if he would exercise even a little, I would eat peas, which I detest. I still haven’t had any reason to eat peas.
I returned to the hospital at 6:30 P.M., armed with a couple of small bottles of water. The physical therapist had told me that lifting the bottles while in bed would be good exercise for Dad. Unfortunately, he wouldn’t touch the bottles. I tried talking with him and shared some of his improved lab results with him, but nothing helped. I even tried to make a deal with him and told him that if he would exercise even a little, I would eat peas, which I detest. I still haven’t had any reason to eat peas. August 3, 2015. It had now been 90 days since Dad first entered the hospital for his seven-to-ten day stay. When Mom and I arrived at 7:45 A.M., Dad’s room was a hubbub of activity. Dr. Phan, the nephrology resident, was assessing him and Emily, his nurse, was exercising his arms and legs. But the first thing that we noticed was Dad’s bed. Yesterday, Dr. Jimenez had told Dad’s nurse that he wanted to see Dad’s bed raised to a more upright position. I had envisioned that the angle of his bed would change from 30 to 75 degrees. What we saw instead was a bed that had morphed into a chair. It played music, automatically adjusted to specific angles, and could change into a chair. Was there anything that this bed couldn’t do?
August 3, 2015. It had now been 90 days since Dad first entered the hospital for his seven-to-ten day stay. When Mom and I arrived at 7:45 A.M., Dad’s room was a hubbub of activity. Dr. Phan, the nephrology resident, was assessing him and Emily, his nurse, was exercising his arms and legs. But the first thing that we noticed was Dad’s bed. Yesterday, Dr. Jimenez had told Dad’s nurse that he wanted to see Dad’s bed raised to a more upright position. I had envisioned that the angle of his bed would change from 30 to 75 degrees. What we saw instead was a bed that had morphed into a chair. It played music, automatically adjusted to specific angles, and could change into a chair. Was there anything that this bed couldn’t do? While Mom and I were at home for dinner, I printed out some recent photos of Dad with the family. I wanted the hospital personnel to see him as more than the sick man that they attended in that hospital bed. He hadn’t entered the hospital as some sickly old man, and I wanted them to have a sense of who he was just a few months earlier. After dinner, Mom and I returned to the hospital around 6:50 P.M. and learned that Dustin was Dad’s nurse. I wasn’t impressed with this nurse, and I wasn’t thrilled to see him again.
While Mom and I were at home for dinner, I printed out some recent photos of Dad with the family. I wanted the hospital personnel to see him as more than the sick man that they attended in that hospital bed. He hadn’t entered the hospital as some sickly old man, and I wanted them to have a sense of who he was just a few months earlier. After dinner, Mom and I returned to the hospital around 6:50 P.M. and learned that Dustin was Dad’s nurse. I wasn’t impressed with this nurse, and I wasn’t thrilled to see him again. I had never heard about procalcitonin (PCT) until today, when Dr. Jimenez mentioned that Dad’s current level was 48—down from 64. As soon as the doctor left the room, I whipped out my iPad and searched the internet for information about PCT. From what I read, a PCT level greater than 10 indicated a “high likelihood of severe sepsis or septic shock.” You didn’t have to be a PhD to know that a PCT level of 48 was pretty bad.
I had never heard about procalcitonin (PCT) until today, when Dr. Jimenez mentioned that Dad’s current level was 48—down from 64. As soon as the doctor left the room, I whipped out my iPad and searched the internet for information about PCT. From what I read, a PCT level greater than 10 indicated a “high likelihood of severe sepsis or septic shock.” You didn’t have to be a PhD to know that a PCT level of 48 was pretty bad. When Dr. Jimenez and his entourage entered the room, he said that Dad was “one tough guy.” He said something about an albumin transfusion (protein) to help with absorption, but I was too excited to remember everything that he said. Mom and I knew that Dad was still in the woods, but we felt that he had finally found the path out. Before the doctor left, he told Melissa, the nurse, that he wanted the bed raised to more of a sitting position. This day also marked the first day since my father’s return that we didn’t hear something about his grave prognosis.
When Dr. Jimenez and his entourage entered the room, he said that Dad was “one tough guy.” He said something about an albumin transfusion (protein) to help with absorption, but I was too excited to remember everything that he said. Mom and I knew that Dad was still in the woods, but we felt that he had finally found the path out. Before the doctor left, he told Melissa, the nurse, that he wanted the bed raised to more of a sitting position. This day also marked the first day since my father’s return that we didn’t hear something about his grave prognosis. Shortly after 10:00 A.M., we met
Shortly after 10:00 A.M., we met  When Dad was transferred from the CCH to Memorial, his flowers could not come with him. Cut flowers and plants are not permitted in the ICU. I had been thinking about it for a couple of days, and I was now determined to brighten up Dad’s room. After lunch, I cleaned the vase that had held his sunflower arrangement, took it back to
When Dad was transferred from the CCH to Memorial, his flowers could not come with him. Cut flowers and plants are not permitted in the ICU. I had been thinking about it for a couple of days, and I was now determined to brighten up Dad’s room. After lunch, I cleaned the vase that had held his sunflower arrangement, took it back to  July 28, 2015. Six days since Dad returned to
July 28, 2015. Six days since Dad returned to  The big surprise of the week occurred right after Dr. White left Dad’s room. During the procession of residents and the attending physician, a woman kept appearing in the doorway, and would then leave. When the room was finally empty of providers, she entered Dad’s room and introduced herself as Aimee from the Patient Relations department. She told us that a hospital employee had contacted her office about Dad, and suggested that she meet with us about the events that led to his return to Memorial. I pulled out my iPad of notes and shared our concerns about some of our interactions with one of the CCH doctors. Aimee told us that they would investigate our complaint and get back to us in 30 days. I assured her that although we had complaints about one person, for the most part, we were pleased with the level of care that Dad had received from his providers. When she left, Mom and I were stunned and kept trying to guess who contacted Aimee’s office.
The big surprise of the week occurred right after Dr. White left Dad’s room. During the procession of residents and the attending physician, a woman kept appearing in the doorway, and would then leave. When the room was finally empty of providers, she entered Dad’s room and introduced herself as Aimee from the Patient Relations department. She told us that a hospital employee had contacted her office about Dad, and suggested that she meet with us about the events that led to his return to Memorial. I pulled out my iPad of notes and shared our concerns about some of our interactions with one of the CCH doctors. Aimee told us that they would investigate our complaint and get back to us in 30 days. I assured her that although we had complaints about one person, for the most part, we were pleased with the level of care that Dad had received from his providers. When she left, Mom and I were stunned and kept trying to guess who contacted Aimee’s office. His pulse was running in the 130s again, and his oxygen saturation levels were low. To compensate for the low oxygen levels, the respiratory therapist increased his oxygen levels on the ventilator to 60%. A few minutes later, the ventilator started alarming, which prompted the nurse to page the respiratory therapist. Evidently, one piece of the ventilator was cross-threaded, which was what caused the system to alarm. The alarms were starting to drive us crazy and I could swear that I could hear them when we were away from the hospital.
His pulse was running in the 130s again, and his oxygen saturation levels were low. To compensate for the low oxygen levels, the respiratory therapist increased his oxygen levels on the ventilator to 60%. A few minutes later, the ventilator started alarming, which prompted the nurse to page the respiratory therapist. Evidently, one piece of the ventilator was cross-threaded, which was what caused the system to alarm. The alarms were starting to drive us crazy and I could swear that I could hear them when we were away from the hospital. When Dr. White and his band of providers arrived outside of Dad’s room, I heard comments about Dad being
When Dr. White and his band of providers arrived outside of Dad’s room, I heard comments about Dad being  Shortly before 4:00 P.M., I was presented with a
Shortly before 4:00 P.M., I was presented with a  Carlos, the dialysis nurse, arrived at 8:15 A.M. and proceeded to prepare Dad for dialysis. At the same time, Dr. Fernandez, one of the
Carlos, the dialysis nurse, arrived at 8:15 A.M. and proceeded to prepare Dad for dialysis. At the same time, Dr. Fernandez, one of the  At 2:15 P.M., the hematology team arrived. Because Dad’s lab work showed that he had
At 2:15 P.M., the hematology team arrived. Because Dad’s lab work showed that he had  Dad’s oxygen levels had been fair, and when Nikita, the respiratory therapist arrived, she increased his oxygen level on the ventilator from 40% to 50%. As she adjusted the ventilator settings, she said that she’d probably decrease the levels back to 40% later in the day.
Dad’s oxygen levels had been fair, and when Nikita, the respiratory therapist arrived, she increased his oxygen level on the ventilator from 40% to 50%. As she adjusted the ventilator settings, she said that she’d probably decrease the levels back to 40% later in the day. July 26, 2015. Mom and I arrived at the hospital shortly after 8:00 A.M.; I looked at Dad, and then over to his IVs. Amazingly, Dad’s night nurse, Tyler, had been able to wean Dad down to one
July 26, 2015. Mom and I arrived at the hospital shortly after 8:00 A.M.; I looked at Dad, and then over to his IVs. Amazingly, Dad’s night nurse, Tyler, had been able to wean Dad down to one  When Dr. White arrived, he acknowledged that while there had been some clinical improvement in my dad’s condition, Dad was still critically ill and his mental status was not improving. To ensure that Dad hadn’t suffered a stroke or a bleed, he planned to order a CT scan. Dr. White restated his concern about Dad’s toes and thought that he probably would lose at least one toe.
When Dr. White arrived, he acknowledged that while there had been some clinical improvement in my dad’s condition, Dad was still critically ill and his mental status was not improving. To ensure that Dad hadn’t suffered a stroke or a bleed, he planned to order a CT scan. Dr. White restated his concern about Dad’s toes and thought that he probably would lose at least one toe. While Mom, Stan, and I were at home for lunch, I decided I would try some music therapy with Dad.
While Mom, Stan, and I were at home for lunch, I decided I would try some music therapy with Dad.