
Saturday, August 15, 2015. Shortly after I arrived at the hospital at 7:45 A.M., Dr. Hayek ordered Dad moved Dad from BiPAP to CPAP support on the ventilator. They then reduced the settings to less support and let him breathe at the lower setting for about 30 minutes before putting him back on the trach collar. The attending physician, Dr. Ghamande, wanted Dad to have at least four hours on the trach collar today. If this trial worked out well, then they would attempt a six-hour trial tomorrow. During the nephrology visit, Dr. Goraya said that it was unlikely that Dad’s kidneys would function again, although they couldn’t say anything definite for another few weeks. Medicare requires that you be on dialysis for 90 days before you can be declared dialysis dependent. Although the 90th day was just around the corner, the nephrologists seemed hesitant to declare that Dad had end-stage renal disease (ESRD) until he reached this milestone.
During my morning update of Dad’s early-morning lab work, I was told that his WBC count had inched up slightly from 10.4 to 10.7. It was still within the normal range, and I was provided the usual song-and-dance routine about how you have to treat the whole patient and not just look at the numbers, but his numbers had not just stopped trending downward, they were moving in the wrong direction. After 102 days, I couldn’t help but worry.
At 9:09 A.M., Pandora, the respiratory therapist, put the trach collar on Dad. He was now breathing on his own again. Leslie, his nurse, then asked him the following three questions to test his mental facilities: 1) Could you hit a nail with a hammer, 2) Can a leaf float on water, 3) Is a one pound rock heavier than a two-pound rock. He did OK on the first two, but answered “sometimes” to the last question.
For the second day in a row, Dad wanted some of our coffee. Mom and I decided that we should quit drinking coffee in front of him. I wondered if he could smell the coffee.
Shortly before 10:00 A.M. Leslie, the nurse, moved Dad into the cardiac chair. At 11:00 A.M., my husband, Stan, texted me that he had arrived from Houston. Mom and I left shortly thereafter to join him for lunch at the house.
After a nice lunch with Stan, Mom and I returned to the hospital at 12:40 P.M., while Stan stayed at the house and did some yard work. Dad was still sitting in the cardiac chair. He kept trying to talk and became pretty frustrated. His breathing trial was over at 1:15 P.M., and Pandora removed the trach collar and moved him to the CPAP setting on the ventilator.
At 1:50 P.M., Leslie rounded up a couple of nurses to help her move Dad from the chair to the bed, where he promptly fell fast asleep sitting up in bed. The ventilator started alarming, which drove Mom crazy. I guess it takes a certain type of alarm to get the attention of a nurse or respiratory therapist. In this case, water had accumulated the lines, which wasn’t life threatening. Unfortunately, we weren’t permitted to touch anything; we just had to listen to and endure the alarm while we watched nurses and aides walk past the room.
At 4:55 P.M., Mom went downstairs to the lobby to meet Stan. I wandered into the hall and happened to meet a nurse that we had dubbed as Daytime Natalie. She was a nurse in the CTICU, and Mom and I were very fond of her. She had a couple of minutes to spare and stopped in to visit with Dad.
Mom, Stan, and I ate dinner at a local restaurant to celebrate Mom’s birthday. Her birthday was tomorrow, but this was Stan’s only night in Temple. After dinner, Mom and Stan went home and I returned to the hospital and met Dad’s night nurse, Janine, and his respiratory therapist, Tatyana. Shortly after I arrived, Dad starting started indicating that he wanted to get out of bed, and continued in earnest until I finally was able to leave around 8:45 P.M. Starting at 8:15 P.M., I had started receiving text messages from Stan, asking if everything was OK with me and Dad. Every time I tried to leave him, he would grab my arm and want me to stay five more minutes. I felt more than just a little guilty when I left.
August 16. Mom’s birthday got off to a nice start with cinnamon rolls and some nice gifts from Stan. As Mom and I were driving to the hospital, my phone rang, but my purse was in the back seat and I couldn’t grab it before the call went to voice mail. I pulled over and noticed that the call was from Scott & White. Leslie, Dad’s nurse, had left a message saying that Dad was very tired and needed to rest. She went on to say that she was a little worried about him this morning and that she had contacted Dr. Stewart, who then put him back on the ventilator. She did not want us to wake him. If Leslie was trying to discourage us from racing to the hospital, she was failing miserably.
We encountered Dr. Goraya on the way into MICU, and she said that they would not be dialyzing Dad today. While talking with Leslie outside of Dad’s room, she said that she had been looking through the last few weeks of Dad’s charts, and by all rights, he should not be here now. Her comment made me feel good about his progress, but his condition was still very fragile.
I called Stan and told him about Leslie’s call, and that I still wanted him to come by the hospital while Mom and I were at church, but that Dad might be sleeping and that Stan should bring something to read. Should Dad wake up, then Stan could interact with him. I also wanted Stan to be with Dad, if the doctors should stop by while Mom and I were attending church.
When church was over, I texted Stan to let him know that Mom and I were heading home. He said that Dad woke up around 11:00 A.M., and that they were stepping him down to the trach collar for another six-hour trial today.
After our lunch, Mom and I arrived at 1:30 P.M. at the hospital and met Stan in the waiting room. He had been shooed out by the nurses about 10 minutes earlier. We were pleased to see that Dad was in the cardiac chair and breathing on his own with the trach collar when we arrived. Dad’s breathing trial started around 1:25 P.M. We had the TV turned on to the PGA tournament. Watching TV might not seem like a milestone, but he had probably watched no more than a couple of hours of TV since he was admitted on May 6. It was nice to see him interested in something.
Mom left the hospital for home around 4:25 P.M. About five minutes after Mom left, Dad finally tired of the breathing trial. He was still on the trach collar when I left at 4:45 P.M. His trial didn’t last much more than three hours, but considering how badly the morning started, we were pleased with his trial.
After dinner, we arrived at Dad’s room at 6:55 P.M. and spoke with Leslie for a few minutes before she left for the day. She said that Dad had been wearing her out. He’d been wiggling down the bed all day, in what seemed like attempts to escape from the bed. She finally made his bed alarm a lot more sensitive so that it would alarm whenever he wiggled down to one end.
Leslie said that she noticed during the day that Dad’s secretions had seemed more yellow and thicker than normal. She said that she had talked to the doctor about ordering a sputum culture. She said that it might not be anything because he’s not running a fever. The WBC count wasn’t collected during the early morning lab work, so I didn’t know if his WBC count was elevated.
Dad’s night nurse was Amanda. When she completed her evening assessment, she told us that his temperature was 98.7, which is practically normal for most people. However, normal for Dad was just over 97 degrees. It probably wasn’t a big deal, but I hoped that the sputum culture tomorrow would reveal something.
August 17. Mom and I arrived at Dad’s room a little after 7:30 A.M. and found that he was restrained and was already receiving conventional dialysis. His nurse, Jasmine, and another nurse were repositioning Dad in his bed, so his curtain was closed. While waiting in the hall I spoke briefly with Amanda, his night nurse, and she said that during her shift, Dad had tried repeatedly to pull out his trach tube. When she explained to him what that would mean, he indicated that he didn’t care and wanted to “be done with it.” To calm him, she gave him some Seroquel. As Dad’s health improved, it seemed that he was his own worst enemy.
Jasmine, Dad’s nurse, later told him that she would remove his restraints if he promised that he would not try to pull out his trach tube. She stressed to him that his safety was her primary concern. He indicated that he would not pull out anything. Jasmine told us that they would put the trach collar on him later today so that he could better express his wishes. Her comment sort of implied that he might get a speaking valve, but I wasn’t sure. I was a little disturbed when I learned that Dad’s WBC count was up to 13.2. Based on Leslie’s comments yesterday and Dad’s elevated WBC count, the doctor had ordered a Bronchoalveolar lavage (BAL) to see if Dad had any new infections.
Dad finally used the letter board and asked lots of questions about his stay. He didn’t realize how long he had been in the hospital and was very surprised when he heard what happened to him. I spent a long time explaining some details about his saga and I think that it helped to improve his attitude. Shortly after that, we started communicating more with the letter board. He seemed to be a lot calmer and seemed to understand more about his circumstances.
Shortly before 11:00 A.M., I told Dad that Mom and I had to leave to attend a meeting with April Jones, the nurse manager at the CCH. We wanted to ensure, or try to ensure, that his second time at the CCH would be better than the first. He seemed pleased and lettered that he would be interested in knowing what she had to say. Following an annoying and frustrating meeting with Ms. Jones and her associates, Mom and I returned home for lunch. I stayed home and worked for the remainder of the afternoon.
When Mom returned to the hospital after lunch, a nun from the hospital’s chaplain office was in Dad’s room singing to him. Using his letter board, Dad told the nun to sing a song to Mom. Dad had already given the nun one of the family photos that I had taped to the wall. She said that she’d hang it in the chapel. Mom found the experience pretty surreal and realized that from one minute to the next, she never knew what to expect from Dad.
After pleading unsuccessfully for days to get Dad to use the letter board, it seemed that he now would not put it down. From what Mom was able to surmise, Dad whipped out the letter board for every person who entered the room—the nurse, doctors, and techs. Using the letter board, he asked Dr. Ambroson to take him to the kitchen, which tickled the doctor. In hindsight, this request was an indication that Dad was having trouble distinguishing the difference between home and the hospital. However, it seemed like a different person was now occupying Dad’s bed.
When Dad’s dialysis session was over, Dawn, the respiratory therapist, put on the trach collar. Then the nurses moved him to the chair. As Mom left the room, Dad used the letter board to tell her to be careful.
When I arrived at Dad’s room at 6:45 P.M., he was still in the cardiac chair, but he was soon moved back to his bed. Dad and I visited until 9:00 P.M. Using the letter board, he asked lots of questions about eating, going home, and many other things. He seemed to have lost some of the clarity that he had during the day, which I attributed to being exhausted from such a busy day. When I left, he still had one more hour remaining on his six-hour trial of the trach collar.
His night nurse, Amanda, said that she would give him some Seroquel this evening after the breathing trial and that he should sleep well. I wasn’t over the moon about Dad’s level of clarity this evening, but he had had quite a day communicating with everyone. I left the hospital hoping that the next day would be even better.



 August 9, 2015. We arrived at the hospital at 9:00 A.M. to find that Dad was still asleep and restrained, the nurse’s name was not on the board, and Dad’s feeding tube was empty. Two out of three of these situations were unacceptable. I went to the nurse’s station to find out who his nurse was and to let them know that his tube feed bottle was empty. A nurse entered the room with a fresh bottle of Nepro, changed out his tubing, and replaced the empty bottle. The nurse also told me that Dad’s nurse was Nicole, who finally showed up at 9:15 A.M. and introduced herself.
August 9, 2015. We arrived at the hospital at 9:00 A.M. to find that Dad was still asleep and restrained, the nurse’s name was not on the board, and Dad’s feeding tube was empty. Two out of three of these situations were unacceptable. I went to the nurse’s station to find out who his nurse was and to let them know that his tube feed bottle was empty. A nurse entered the room with a fresh bottle of Nepro, changed out his tubing, and replaced the empty bottle. The nurse also told me that Dad’s nurse was Nicole, who finally showed up at 9:15 A.M. and introduced herself.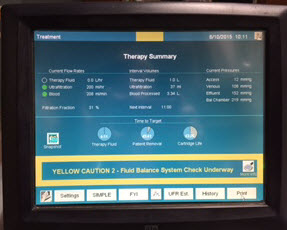 August 10. We arrived at 7:40 A.M. and noticed that Dad was already on dialysis. Before we arrived, they had drawn blood and ran an
August 10. We arrived at 7:40 A.M. and noticed that Dad was already on dialysis. Before we arrived, they had drawn blood and ran an 

 August 7, 2015. Mom and I arrived at the hospital at 7:45 A.M. Dad was still receiving CPAP breathing support. We were surprised to see that he was not having dialysis, but we had scarcely put down our purses when Lucy, the dialysis nurse, stopped by and said that she had been told to set up the (traditional) four-hour dialysis session. As she left the room,
August 7, 2015. Mom and I arrived at the hospital at 7:45 A.M. Dad was still receiving CPAP breathing support. We were surprised to see that he was not having dialysis, but we had scarcely put down our purses when Lucy, the dialysis nurse, stopped by and said that she had been told to set up the (traditional) four-hour dialysis session. As she left the room,  August 8. Mom and I arrived at Dad’s room at 6:30 A.M. The room was dark and Dad was still sleeping. Jennifer, his nurse, arrived at 7:30 A.M. and started her morning assessment of Dad. When she was finished, she told us that the night nurse told her that Dad was very agitated during the night. I wasn’t sure what that meant, but it didn’t sound good. On a more positive note, Dad’s WBC count was still trending downward.
August 8. Mom and I arrived at Dad’s room at 6:30 A.M. The room was dark and Dad was still sleeping. Jennifer, his nurse, arrived at 7:30 A.M. and started her morning assessment of Dad. When she was finished, she told us that the night nurse told her that Dad was very agitated during the night. I wasn’t sure what that meant, but it didn’t sound good. On a more positive note, Dad’s WBC count was still trending downward. August 5, 2015. When Mom and I arrived this morning, Dr. Brett Ambroson, the resident, was finishing up his morning assessment of Dad’s current status. We were pleased to learn that the vomiting episodes from the previous day had stopped. Dr. Ambroson also noted that Dad would now move his extremities when prompted by him or the other care providers. When I asked about Dad’s WBC count, the doctor said that it was down slightly from yesterday. I wasn’t thrilled with the very slight decrease, but at least the steady upward trend had been arrested. While speaking with Dr. Ambroson, Lucy and Cheryl, the dialysis nurse and her aide, prepared Dad for another eight-hour session.
August 5, 2015. When Mom and I arrived this morning, Dr. Brett Ambroson, the resident, was finishing up his morning assessment of Dad’s current status. We were pleased to learn that the vomiting episodes from the previous day had stopped. Dr. Ambroson also noted that Dad would now move his extremities when prompted by him or the other care providers. When I asked about Dad’s WBC count, the doctor said that it was down slightly from yesterday. I wasn’t thrilled with the very slight decrease, but at least the steady upward trend had been arrested. While speaking with Dr. Ambroson, Lucy and Cheryl, the dialysis nurse and her aide, prepared Dad for another eight-hour session. I returned to the hospital at 6:30 P.M., armed with a couple of small bottles of water. The physical therapist had told me that lifting the bottles while in bed would be good exercise for Dad. Unfortunately, he wouldn’t touch the bottles. I tried talking with him and shared some of his improved lab results with him, but nothing helped. I even tried to make a deal with him and told him that if he would exercise even a little, I would eat peas, which I detest. I still haven’t had any reason to eat peas.
I returned to the hospital at 6:30 P.M., armed with a couple of small bottles of water. The physical therapist had told me that lifting the bottles while in bed would be good exercise for Dad. Unfortunately, he wouldn’t touch the bottles. I tried talking with him and shared some of his improved lab results with him, but nothing helped. I even tried to make a deal with him and told him that if he would exercise even a little, I would eat peas, which I detest. I still haven’t had any reason to eat peas. August 3, 2015. It had now been 90 days since Dad first entered the hospital for his seven-to-ten day stay. When Mom and I arrived at 7:45 A.M., Dad’s room was a hubbub of activity. Dr. Phan, the nephrology resident, was assessing him and Emily, his nurse, was exercising his arms and legs. But the first thing that we noticed was Dad’s bed. Yesterday, Dr. Jimenez had told Dad’s nurse that he wanted to see Dad’s bed raised to a more upright position. I had envisioned that the angle of his bed would change from 30 to 75 degrees. What we saw instead was a bed that had morphed into a chair. It played music, automatically adjusted to specific angles, and could change into a chair. Was there anything that this bed couldn’t do?
August 3, 2015. It had now been 90 days since Dad first entered the hospital for his seven-to-ten day stay. When Mom and I arrived at 7:45 A.M., Dad’s room was a hubbub of activity. Dr. Phan, the nephrology resident, was assessing him and Emily, his nurse, was exercising his arms and legs. But the first thing that we noticed was Dad’s bed. Yesterday, Dr. Jimenez had told Dad’s nurse that he wanted to see Dad’s bed raised to a more upright position. I had envisioned that the angle of his bed would change from 30 to 75 degrees. What we saw instead was a bed that had morphed into a chair. It played music, automatically adjusted to specific angles, and could change into a chair. Was there anything that this bed couldn’t do? While Mom and I were at home for dinner, I printed out some recent photos of Dad with the family. I wanted the hospital personnel to see him as more than the sick man that they attended in that hospital bed. He hadn’t entered the hospital as some sickly old man, and I wanted them to have a sense of who he was just a few months earlier. After dinner, Mom and I returned to the hospital around 6:50 P.M. and learned that Dustin was Dad’s nurse. I wasn’t impressed with this nurse, and I wasn’t thrilled to see him again.
While Mom and I were at home for dinner, I printed out some recent photos of Dad with the family. I wanted the hospital personnel to see him as more than the sick man that they attended in that hospital bed. He hadn’t entered the hospital as some sickly old man, and I wanted them to have a sense of who he was just a few months earlier. After dinner, Mom and I returned to the hospital around 6:50 P.M. and learned that Dustin was Dad’s nurse. I wasn’t impressed with this nurse, and I wasn’t thrilled to see him again. Shortly after 10:00 A.M., we met
Shortly after 10:00 A.M., we met  When Dad was transferred from the CCH to Memorial, his flowers could not come with him. Cut flowers and plants are not permitted in the ICU. I had been thinking about it for a couple of days, and I was now determined to brighten up Dad’s room. After lunch, I cleaned the vase that had held his sunflower arrangement, took it back to
When Dad was transferred from the CCH to Memorial, his flowers could not come with him. Cut flowers and plants are not permitted in the ICU. I had been thinking about it for a couple of days, and I was now determined to brighten up Dad’s room. After lunch, I cleaned the vase that had held his sunflower arrangement, took it back to  His pulse was running in the 130s again, and his oxygen saturation levels were low. To compensate for the low oxygen levels, the respiratory therapist increased his oxygen levels on the ventilator to 60%. A few minutes later, the ventilator started alarming, which prompted the nurse to page the respiratory therapist. Evidently, one piece of the ventilator was cross-threaded, which was what caused the system to alarm. The alarms were starting to drive us crazy and I could swear that I could hear them when we were away from the hospital.
His pulse was running in the 130s again, and his oxygen saturation levels were low. To compensate for the low oxygen levels, the respiratory therapist increased his oxygen levels on the ventilator to 60%. A few minutes later, the ventilator started alarming, which prompted the nurse to page the respiratory therapist. Evidently, one piece of the ventilator was cross-threaded, which was what caused the system to alarm. The alarms were starting to drive us crazy and I could swear that I could hear them when we were away from the hospital. When Dr. White and his band of providers arrived outside of Dad’s room, I heard comments about Dad being
When Dr. White and his band of providers arrived outside of Dad’s room, I heard comments about Dad being  Shortly before 4:00 P.M., I was presented with a
Shortly before 4:00 P.M., I was presented with a  Carlos, the dialysis nurse, arrived at 8:15 A.M. and proceeded to prepare Dad for dialysis. At the same time, Dr. Fernandez, one of the
Carlos, the dialysis nurse, arrived at 8:15 A.M. and proceeded to prepare Dad for dialysis. At the same time, Dr. Fernandez, one of the  At 2:15 P.M., the hematology team arrived. Because Dad’s lab work showed that he had
At 2:15 P.M., the hematology team arrived. Because Dad’s lab work showed that he had  Dad’s oxygen levels had been fair, and when Nikita, the respiratory therapist arrived, she increased his oxygen level on the ventilator from 40% to 50%. As she adjusted the ventilator settings, she said that she’d probably decrease the levels back to 40% later in the day.
Dad’s oxygen levels had been fair, and when Nikita, the respiratory therapist arrived, she increased his oxygen level on the ventilator from 40% to 50%. As she adjusted the ventilator settings, she said that she’d probably decrease the levels back to 40% later in the day. July 24, 2015. The call that we dreaded from the hospital during the night hadn’t come.
July 24, 2015. The call that we dreaded from the hospital during the night hadn’t come. 
 Mom and I went home for dinner and returned to the hospital at 7:15 P.M. Charlie, the respiratory therapist, had just finished Dad’s trach and oral care and ventilator maintenance. Dad was still on three vasopressors. Mom and I met Donna, the night nurse, before leaving for the night. She told us that Dad had additional blood draw after dialysis and that his WBC count was now 22.7, up another 4 points from this morning. His WBC count hadn’t increased at this rate since
Mom and I went home for dinner and returned to the hospital at 7:15 P.M. Charlie, the respiratory therapist, had just finished Dad’s trach and oral care and ventilator maintenance. Dad was still on three vasopressors. Mom and I met Donna, the night nurse, before leaving for the night. She told us that Dad had additional blood draw after dialysis and that his WBC count was now 22.7, up another 4 points from this morning. His WBC count hadn’t increased at this rate since  Now that Dad was back on the ventilator, he couldn’t talk. I got some wild idea yesterday that I had to give Dad a chance to communicate with us if he was going to die. Andrea said that she would contact the respiratory therapist to see if it would be possible to enable him to talk. The respiratory therapist contacted Svenja, the Trach Goddess of Scott & White. We hadn’t seen her since June, when she first
Now that Dad was back on the ventilator, he couldn’t talk. I got some wild idea yesterday that I had to give Dad a chance to communicate with us if he was going to die. Andrea said that she would contact the respiratory therapist to see if it would be possible to enable him to talk. The respiratory therapist contacted Svenja, the Trach Goddess of Scott & White. We hadn’t seen her since June, when she first