October 26, 2015. I had hoped that we’d have an uneventful night, but shortly after 1:00 A.M. Dad started coughing. I could hear Michell encouraging him to use the Yankauer wand, but he refused and kept coughing that terrible wet cough. I finally got up and went downstairs to see if I could convince him to use it, but at 2:00 A.M. I opened a trach care kit, suctioned his secretions, and then returned to bed. When my iPhone alarm played its annoying wake-up ring tone at 3:30 A.M., I was too tired to get out of bed. I kept snoozing the alarm until 4:15 A.M. and started to work 15 minutes later with a much-needed cup of coffee.
Dad was slow to wake up this morning, too, which was OK for him because he didn’t have any early appointments. At 7:00 A.M. he was ready for me to administer his morning trach care and meds.
In addition to work, I had several administrative health care chores to address today. After 27 days at home, we were running low on meds, so I emailed Dr. Issac to have him order new prescriptions. I also needed to reschedule Dad’s wound care appointment. I don’t know what I had been thinking, but when this appointment was scheduled, I didn’t realize that it could conflict with Dad’s dialysis if we encountered any glitches with the dialysis session or transportation. Also, within the next few days, Dad would require a 30-day physical therapy assessment, which I scheduled with Kathleen.
When I had logged on to Dad’s My Chart medical portal account over the weekend, I had learned that thanks to a referral from Dr. Issac, Dad now had an appointment with a pulmonologist. Unfortunately, the appointment was scheduled for January 4, more than two months from now. When I called to see if I could schedule an earlier appointment, I learned that they were booked solid until the new year. I guess that explained the January 4 date, and that I wasn’t going to do any better.
We were running very low on Nepro. When I called American HomePatient to order more, the clerk asked me about the other items that I needed. I told her that I didn’t know what all I needed and was informed that I was supposed to place a single order for everything that I would need for the upcoming month. I had once told Dr. White that patients and family needed a playbook to understand how to navigate the hospital system. The same was true for home health care. The American HomePatient folks were very friendly, but a short bulleted list of guidelines, not to mention an order form, would have been very helpful.
My final call for Dad was to Scott & White Home Care to see how long we were covered by Medicare. I learned that we had received an initial 60 days of coverage. At the end of the 60 days, Dad would be reassessed for an additional 60 days of coverage. This was good information to know and it would have been nice to know it about 30 days earlier.
While I was working, Stephanie, a new nurse, arrived to check on Dad. Because she had not been here before, she performed a very thorough assessment of him, which I learned was the typical protocol for all first visits. After she left, Michell told me that Stephanie had also changed Dad’s trach dressing, which made me feel as uncomfortable as the time that my mother-in-law cleaned out my refrigerator. I should have administered Dad’s midday trach care and changed his dressing an hour earlier, but I hadn’t been able to take a break.
Several days earlier, our neighbor Barbara, had brought Dad some flowers and cake. Mom called Barbara to see if she could return her cake holder. While they were talking, Barbara asked about Dad’s condition and if he was swallowing yet. Mom told her, no, and then explained that we needed a referral from a pulmonologist, but we wouldn’t be able to see one until January 4. She and her husband are both doctors at Scott & White and Barbara said that she could help. Mom and I were hopeful that we might be able to expedite the process.
I was bone tired today, but I managed to eke out eight hours of work and sneak in a little nap. When I woke up, Mom and I drove to the HOP office to fill out an application for a paratransit pass for Dad. Their office was less than 10 miles from my parents’ home, and we thought that we could expedite this process by filling out the form in person. Unlike some websites that enabled you to download a PDF version of the application form, this one required you to request that they send you one by mail.
When Mom and I returned home shortly before 5:00 P.M., Dad was napping. We woke him for happy hour, but he said that happy hour wasn’t that much fun for him, and he went to his room to read the paper. He stayed there until Mom, Michell, and I had finished dinner. I knew that two days didn’t constitute a trend, but now Dad had seemed depressed for two days. Thankfully, he still wanted to play Oh Hell when we finished dinner. Michell won for the first time, but Dad was a close second.
We got Dad snug in bed by 8:30 P.M. He had suctioned himself pretty well while he was getting ready and I didn’t encounter any secretions during the nighttime trach care. I hoped that this was a positive sign for a good night’s sleep.
October 27. It was becoming apparent to me that I was clueless when it came to predicting good and bad nights for Dad. Although he seemed fine when he went to bed, within four hours, secretions had accumulated in his trach. As usual, he wasn’t too keen on suctioning himself at night. This combination of secretion build-up and his refusal to suction led to lots of uncomfortable coughing. Around 2:00 A.M, I heard him call for help. I ran downstairs and he said that he needed the urinal. It’s supposed to be placed on the bedrail, but tonight it was left in the bathroom. He hadn’t wanted to bother anyone, so he tried to get out of bed to get it and was partly out of bed when I entered the room. After Michell and I moved him back into bed, I trudged back upstairs to bed for a bit more sleep.
Michell and I woke Dad at 4:30 A.M. I took care of his trach and then Michell took over. He was ready to go by 5:45 A.M., but after we had waited for several minutes past his scheduled pickup time, I called the dispatch office to check on their status. They never answered the phone, but they eventually arrived shortly before 6:30 A.M.
A few hours later, I contacted Sue, the nurse practitioner at the dialysis center, and asked her about my request for Dad’s prescriptions. She hadn’t seen my earlier email to Dr. Issac and promised to place the new orders at once.
Although Dad had less fluid removed today than on Saturday, he was exhausted when he returned from the dialysis center. After I administered his midday meds and trach care, he slept for three hours. He was awake and ready to get up shortly after I logged off from work for the day, and he joined us for happy hour. He returned to his room while we ate dinner, and he was ready for a game of Oh Hell when we were finished. Mom was the big winner tonight, and once again, Dad came in second place.
October 28. Dad had another night of coughing. I got up a couple of times to check on him, but he seemed to be sleeping through it. I swear he could sleep through just about anything. I got up at 3:30 A.M. and started to work at 3:45 A.M. After several weeks working these crazy hours, my coworkers in India, Israel, and the UK had become accustomed to seeing me online a couple of hours earlier than usual. Depending on the location, they were now seeing me online during their morning to early afternoon instead of late afternoon to early evening. As nice as it was to have more time to meet with them, I hoped that we wouldn’t continue this schedule much longer. As convenient as my hours were for my coworkers to the east of me, it wasn’t as convenient for those to the west, like my manager, who worked in California. I was very lucky to have a job that enabled me to work while taking care of a family member.
Today was an off day for dialysis, so Dad didn’t need to wake up before 5:00 A.M. During a break from work, I took care of the trach care and meds, and then left him to Michell. During one of my meetings, Gale arrived and Michell updated her on the events of the past seven days.
Stephanie, the nurse, stopped by again today. I was concerned about Dad’s secretions and was afraid that he was still battling pneumonia. In addition to the suctioning at night and during trach care, he also suctioned himself with the Yankauer wand during the day. She listened to his chest and said that it was clear. She explained that the trach alone was enough to cause secretions and that the effects of pneumonia can last for months. He had a lot of issues, but she thought that he was progressing well on all fronts, except for the bed sore.
Kathleen, the physical therapist, came by and performed her 30-day assessment of Dad and formulated a new plan for the next 30 days. In the coming month, Dad’s goals would include transfers to the shower and the dialysis chair. Dad needed to be able to maneuver from a wheelchair to the dialysis chair so that we could change from the expensive ambulance transfer to the more affordable HOP paratransit bus. I was still nervous about Medicare coverage for the various therapies, including speech therapy, which hadn’t yet started. Kathleen assured me that if Dad progressed well in one area but not as well in others, Medicare wouldn’t stop all of the services—only those no longer necessary.
While I was still working, Mom went to the drug store to pick up Dad’s prescriptions. In the short time that she was at the pharmacy, her car battery died. Fortunately, I was a member of AAA and eventually she received service and was able to start the car and drive home.
During the afternoon, Dad was up for most of the day and joined us for happy hour, but rested while Mom, Gale, and I ate dinner. Gale mentioned to me that although he seemed physically better, she thought that Dad seemed sad. I didn’t want to hear comments like this because they only reinforced my concerns about him and reminded me of articles that I had read about occurrences of depression following ICU delirium.
We played cards again, and Mom won again. We started moving Dad toward the bedroom and his nighttime ritual at 8:15 P.M.
October 29. The alarm woke me this morning at 3:30 A.M. Having the alarm wake me instead of Dad was like a gift. It seemed that I had slept throughout the night—6 hours! I got up at 3:45 A.M., started the coffee maker, and was working by 4:00 A.M. Gale started waking Dad around 4:15 A.M. During trach care this morning, Dad gave me a good scare when he had a hard coughing jag while I was suctioning him. He seemed to get over it without any damage, except to my blood pressure. With a little assistance from Gale and me, Dad was ready to go at 5:45 A.M. While we were waiting for the ambulance he scared the bejeezus out of me again when he experienced another hard coughing spell. We had come too far for him to slip away from us again. He hadn’t coughed like this since he had been home, and few things scared me as much as these hard coughing spells.
This morning, the ambulance drivers were both women, which was a first for us. Dad’s blood pressure dropped during dialysis, so they stopped removing fluid early and just cleaned his blood. In the end, they removed about 820 ml—about half of the usual amount. The ambulance arrived at noon to bring Dad home, and surprisingly, the same two EMTs from the morning also brought him home. It was unusual to have the same EMTs on both ends of the trip. It was more unusual that both EMTs were women.
Dad was very tired when he arrived home and he needed more than the usual assistance to transfer him from the gurney to the wheelchair. Shortly after administering his midday meds and trach care, he was out like a light for three hours. One of my weekly chores was to keep the pill dispenser full. During my lunch break, I organized pills and called Sue for a couple more refills. It would have been nice if all of the prescriptions lasted the same length of time. By the time that I logged off for the day, I had worked for almost 10 hours, and I was wiped out.
We were experiencing Chamber-of-Commerce-type weather today and the four of us agreed that the patio was perfect for happy hour. The temperature hovered around 80 degrees Fahrenheit, with low humidity. We sat out on the patio for about an hour. After dinner, we were all ready for a game of cards—especially Mom, who won again. She seemed to be on a roll.
I had some trouble suctioning Dad tonight. It seemed that the tubing that I used to suction the trach kept hitting something, and I silently reprimanded myself for not changing his trach today. I don’t like to change out the trach on dialysis days, and now I was very tired, too. However, the thought that his airway might become obstructed during the night made it difficult for me to go to sleep, and I kept waking up because I couldn’t hear him through the baby monitor.
Good grief. I couldn’t sleep when he was coughing and I couldn’t sleep when he was quiet.




 After lunch, Dad had Mom and Gale take him outside to check on the hoses in the backyard. My parents’ acre lot had quite a few young trees. Dad had set up permanent irrigation to some of the trees, but his system required that some hoses be moved among the trees. Diane had been his ready assistant a few days ago, and now it was Gale’s turn. Fortunately, Gale loved being outdoors.
After lunch, Dad had Mom and Gale take him outside to check on the hoses in the backyard. My parents’ acre lot had quite a few young trees. Dad had set up permanent irrigation to some of the trees, but his system required that some hoses be moved among the trees. Diane had been his ready assistant a few days ago, and now it was Gale’s turn. Fortunately, Gale loved being outdoors. In addition to being concerned about all of the time that Dad was off of the humidified air, I was also concerned about the considerable amount of time he spent disconnected from his tube feed. The tube feed was available to him only in his room because his wheelchair had no IV pole to which to attach the Kangaroo pump that operated the feed. I suspected that he was receiving less than half of the protein and other nutrients that he needed. If I could attach the Kangaroo pump to the wheelchair, then he could receive nutrition all the time as he moved around the house, property, and elsewhere, except during dialysis. When I had called
In addition to being concerned about all of the time that Dad was off of the humidified air, I was also concerned about the considerable amount of time he spent disconnected from his tube feed. The tube feed was available to him only in his room because his wheelchair had no IV pole to which to attach the Kangaroo pump that operated the feed. I suspected that he was receiving less than half of the protein and other nutrients that he needed. If I could attach the Kangaroo pump to the wheelchair, then he could receive nutrition all the time as he moved around the house, property, and elsewhere, except during dialysis. When I had called  During the past few days, I had been discovering some of the flaws in the homecare system and Medicare. When the nurse encouraged us to take Dad to a wound care specialist, I called the nurse practitioner at the CCH for the referral and was told that Dad was no longer their patient and that we would have to get all of our referrals from his primary care physician (PCP). Dad had been hospitalized since May and hadn’t seen his PCP in almost two years. As a matter of fact, we had to cancel an appointment with her during his hospitalization. When I called the office of Dr. Sarla Patil, his PCP, and explained our predicament to her nurse, she said that the doctor could not provide any referrals or refill his prescriptions unless he came to her office. She went on to say that had Dr. Patil been the referring physician for homecare, then they could help, which was a nonhelpful and ridiculous comment. When I explained that he wasn’t ambulatory, she apologized and said that there was nothing that she could do. In desperation, I called the office of the doctor who had saved his life, Dr. Randall Smith. I spoke with his nurse, Christine, and explained Dad’s
During the past few days, I had been discovering some of the flaws in the homecare system and Medicare. When the nurse encouraged us to take Dad to a wound care specialist, I called the nurse practitioner at the CCH for the referral and was told that Dad was no longer their patient and that we would have to get all of our referrals from his primary care physician (PCP). Dad had been hospitalized since May and hadn’t seen his PCP in almost two years. As a matter of fact, we had to cancel an appointment with her during his hospitalization. When I called the office of Dr. Sarla Patil, his PCP, and explained our predicament to her nurse, she said that the doctor could not provide any referrals or refill his prescriptions unless he came to her office. She went on to say that had Dr. Patil been the referring physician for homecare, then they could help, which was a nonhelpful and ridiculous comment. When I explained that he wasn’t ambulatory, she apologized and said that there was nothing that she could do. In desperation, I called the office of the doctor who had saved his life, Dr. Randall Smith. I spoke with his nurse, Christine, and explained Dad’s  October 15. At 1:30 A.M., I was awakened by the sound of coughing coming through the baby monitor. I kept hoping that Dad would use the
October 15. At 1:30 A.M., I was awakened by the sound of coughing coming through the baby monitor. I kept hoping that Dad would use the  trach bib moistened with sterile water to provide some moisture to his lungs, he no longer was deprived of tube feed when he left the bedroom. Dad had to be more careful as he navigated the hallways to ensure that the pump didn’t hit the wall or knock photographs off of the wall.
trach bib moistened with sterile water to provide some moisture to his lungs, he no longer was deprived of tube feed when he left the bedroom. Dad had to be more careful as he navigated the hallways to ensure that the pump didn’t hit the wall or knock photographs off of the wall.
 After Paula left, Dad napped for about 2-1/2 hours. By the time that he woke up, Mom, Gale, and I had eaten dinner. It had now been a week since I had changed Dad’s trach. I wanted to change it again before bedtime and before Gale ended her week with us. During normal trach care, I’d set up a TV tray next to the bed and lay out the contents of the kit. For the trach change, I grabbed another TV tray and set up the changing kit. I mentally ran through the changing routine a couple of times, took a breath, and got started. After donning the gloves, I attached the trach collar to the new trach, applied the lubricant to the trach, loosened the obturator and told Gale to make sure that I pulled it out after I inserted the trach. Trach tubes are very flexible, and the obturator provides the stiffness necessary to insert the trach. If I didn’t remove the obturator, then Dad couldn’t breathe. Now that the new
After Paula left, Dad napped for about 2-1/2 hours. By the time that he woke up, Mom, Gale, and I had eaten dinner. It had now been a week since I had changed Dad’s trach. I wanted to change it again before bedtime and before Gale ended her week with us. During normal trach care, I’d set up a TV tray next to the bed and lay out the contents of the kit. For the trach change, I grabbed another TV tray and set up the changing kit. I mentally ran through the changing routine a couple of times, took a breath, and got started. After donning the gloves, I attached the trach collar to the new trach, applied the lubricant to the trach, loosened the obturator and told Gale to make sure that I pulled it out after I inserted the trach. Trach tubes are very flexible, and the obturator provides the stiffness necessary to insert the trach. If I didn’t remove the obturator, then Dad couldn’t breathe. Now that the new  trach tube was ready, I removed the ties on his trach collar and then removed the trach from his throat, placed it on one of the TV trays, picked up the sterile trach tube, and inserted it. Because I was holding my breath and counting in my head, I knew that I had made the change in less than 8 seconds. Gale reminded me to remove the obturator, and Dad coughed up a huge wad of secretion, which I had been told was a good thing because it meant that the trach tube was properly placed.
trach tube was ready, I removed the ties on his trach collar and then removed the trach from his throat, placed it on one of the TV trays, picked up the sterile trach tube, and inserted it. Because I was holding my breath and counting in my head, I knew that I had made the change in less than 8 seconds. Gale reminded me to remove the obturator, and Dad coughed up a huge wad of secretion, which I had been told was a good thing because it meant that the trach tube was properly placed. October 6. Today was a special day because it was Dad’s 87th birthday. Just
October 6. Today was a special day because it was Dad’s 87th birthday. Just 

 I had just a limited supply of the trach kits from Angela, so I used the information on the packaging to search online for a provider. I found the kits at a company called Healthcare Supply Pros, and ordered two cases, each case containing 36 kits. The order set me back $130.00, but these kits would appreciably lower my aggravation and stress levels, so I felt that the expense was worth it. I just hoped that my order would arrive before I ran through my supply of appropriate kits. It was a shame that we had six cases of the trach care kits from AHP.
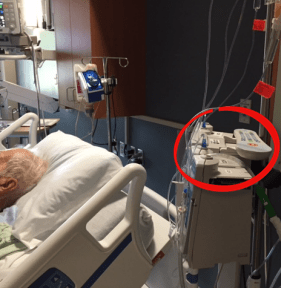
I had just a limited supply of the trach kits from Angela, so I used the information on the packaging to search online for a provider. I found the kits at a company called Healthcare Supply Pros, and ordered two cases, each case containing 36 kits. The order set me back $130.00, but these kits would appreciably lower my aggravation and stress levels, so I felt that the expense was worth it. I just hoped that my order would arrive before I ran through my supply of appropriate kits. It was a shame that we had six cases of the trach care kits from AHP. monitors used to trigger alarms for dangerous blood pressure readings. To calculate it, you multiply the systolic (top) number by two, add the product to the diastolic (bottom) number, and then divide by three. In the hospital, the monitor triggered a piercing alarm when the number dipped below 65 (or 60 during dialysis). I quickly performed the calculations, and his MAP was 42, which triggered my own internal alarm. We hadn’t been taking care of Dad for 24 hours and I suddenly felt like the failure that the medical experts thought we would be. In a panic, I called the Home Care office, gave them Dad’s blood pressure reading, and was instructed to call 911. The few minutes that it took for the ambulance to arrive seemed like an hour. When the EMTs arrived, they took Dad’s vitals and found them to be normal. They stayed for a few minutes and checked his blood pressure again. They told us that they could transport Dad to the hospital, but said us that if Dad was their relative, they’d keep him at home and call 911 again if we had more problems. We happily accepted their advice and thanked them as they left.
monitors used to trigger alarms for dangerous blood pressure readings. To calculate it, you multiply the systolic (top) number by two, add the product to the diastolic (bottom) number, and then divide by three. In the hospital, the monitor triggered a piercing alarm when the number dipped below 65 (or 60 during dialysis). I quickly performed the calculations, and his MAP was 42, which triggered my own internal alarm. We hadn’t been taking care of Dad for 24 hours and I suddenly felt like the failure that the medical experts thought we would be. In a panic, I called the Home Care office, gave them Dad’s blood pressure reading, and was instructed to call 911. The few minutes that it took for the ambulance to arrive seemed like an hour. When the EMTs arrived, they took Dad’s vitals and found them to be normal. They stayed for a few minutes and checked his blood pressure again. They told us that they could transport Dad to the hospital, but said us that if Dad was their relative, they’d keep him at home and call 911 again if we had more problems. We happily accepted their advice and thanked them as they left. I-35, the interstate highway that is the primary route between Dallas and Temple, is notorious for bad accidents that shut down the freeway. Becky was a victim of such a shutdown and arrived about three hours late at 7:30 P.M. Following her arrival, Gale and I transferred Dad to his wheelchair and wheeled him out to our patio where the four of us visited with Becky for about 30 minutes.
I-35, the interstate highway that is the primary route between Dallas and Temple, is notorious for bad accidents that shut down the freeway. Becky was a victim of such a shutdown and arrived about three hours late at 7:30 P.M. Following her arrival, Gale and I transferred Dad to his wheelchair and wheeled him out to our patio where the four of us visited with Becky for about 30 minutes. At 8:30 P.M., Gale started preparing Dad for bed. After he was in bed, I administered the meds and trach care. While I was busy with Dad, Gale changed out the tube feed bags, which had to be changed every 24 hours. Dad hated to be without his speaking valve, so I broke with one of Angela’s rules and left it in place during the night. If he needed help, we needed to be able to hear him. He complained when I removed the speaking valve during trach care. I knew that I’d never hear the end of it if I removed it overnight.
At 8:30 P.M., Gale started preparing Dad for bed. After he was in bed, I administered the meds and trach care. While I was busy with Dad, Gale changed out the tube feed bags, which had to be changed every 24 hours. Dad hated to be without his speaking valve, so I broke with one of Angela’s rules and left it in place during the night. If he needed help, we needed to be able to hear him. He complained when I removed the speaking valve during trach care. I knew that I’d never hear the end of it if I removed it overnight.
 After Jennifer left the room, Dad asked me about “all of the buildings that he was going to travel through.” I explained to him that to get home, he wouldn’t travel through buildings, but that his ambulance would take him home via the Loop and 31st Street. I drew him a bad, oversimplified map of the area and explained where everything was and the distances between them. He had been hospitalized so long that he was confused, thinking that there was a difference between our house and our home. He then told me that it would be prudent to get him a bedpan, so I called the nurse and left his room.
After Jennifer left the room, Dad asked me about “all of the buildings that he was going to travel through.” I explained to him that to get home, he wouldn’t travel through buildings, but that his ambulance would take him home via the Loop and 31st Street. I drew him a bad, oversimplified map of the area and explained where everything was and the distances between them. He had been hospitalized so long that he was confused, thinking that there was a difference between our house and our home. He then told me that it would be prudent to get him a bedpan, so I called the nurse and left his room. At 11:00 A.M., Angela returned, and my respiratory therapy training ratcheted up a notch. In addition to suctioning Dad today, she said that I would
At 11:00 A.M., Angela returned, and my respiratory therapy training ratcheted up a notch. In addition to suctioning Dad today, she said that I would  While I was sitting with Dad, Angela returned to the room with printed instructions about how to suction and change out a trach. Dad was sleeping, so I decided to read the entire document. I write technical documentation for a living, and although I’m not diligent about always reading it, this seemed like a good time to read the manual. I was glad that I did. When Angela stopped by again, I told her that the two other respiratory therapists had had me insert the tubing much further into Dad’s trach than the instructions advised. She told me that she had noticed that I had performed deep suctioning on Dad, but that it wasn’t necessary. When I changed my suctioning technique, I found that suctioning didn’t hurt Dad the way it did with some of the respiratory therapists. I was glad that Angela was now my trainer. I recalled how Dad had told her that she was different from the other respiratory therapists and how he didn’t like others, like Victor. Angela had me suction Dad the rest of the day, and by the end of the day, I was somewhat comfortable with the procedure, although I still had to psych myself up for it.
While I was sitting with Dad, Angela returned to the room with printed instructions about how to suction and change out a trach. Dad was sleeping, so I decided to read the entire document. I write technical documentation for a living, and although I’m not diligent about always reading it, this seemed like a good time to read the manual. I was glad that I did. When Angela stopped by again, I told her that the two other respiratory therapists had had me insert the tubing much further into Dad’s trach than the instructions advised. She told me that she had noticed that I had performed deep suctioning on Dad, but that it wasn’t necessary. When I changed my suctioning technique, I found that suctioning didn’t hurt Dad the way it did with some of the respiratory therapists. I was glad that Angela was now my trainer. I recalled how Dad had told her that she was different from the other respiratory therapists and how he didn’t like others, like Victor. Angela had me suction Dad the rest of the day, and by the end of the day, I was somewhat comfortable with the procedure, although I still had to psych myself up for it. If you spend any time at a hospital, you quickly learn that healthcare is a dirty business and the floor is difficult to keep clean. My parents’ house, including their bedroom, was carpeted with a beautiful sea green carpet. We were pretty certain that the carpeting would not survive Dad’s home care. One of Stan’s assignments was to figure out how to save the carpet. He eventually decided on chair mats. He bought out the supply of rectangular mats at Staples and Office Max and then worked out the arrangement of the mats in the bedroom. In addition to protecting the floor, the mats provided a relatively hard surface and protected the carpet from some of the heavy equipment and the wheelchair that would be brought into the room. He also purchased some shelving and boxes that we would need for storing medical supplies. Thank goodness my parents’ bedroom was large enough to accommodate everything.
If you spend any time at a hospital, you quickly learn that healthcare is a dirty business and the floor is difficult to keep clean. My parents’ house, including their bedroom, was carpeted with a beautiful sea green carpet. We were pretty certain that the carpeting would not survive Dad’s home care. One of Stan’s assignments was to figure out how to save the carpet. He eventually decided on chair mats. He bought out the supply of rectangular mats at Staples and Office Max and then worked out the arrangement of the mats in the bedroom. In addition to protecting the floor, the mats provided a relatively hard surface and protected the carpet from some of the heavy equipment and the wheelchair that would be brought into the room. He also purchased some shelving and boxes that we would need for storing medical supplies. Thank goodness my parents’ bedroom was large enough to accommodate everything. Shortly after we arrived, I went to the nurses’ station to see Jennifer. She said that she had been waiting for me to arrive so that I could administer Dad’s morning meds. At practically the same time, Dr. Smith arrived and we discussed Dad’s feeding tube and his invasive lines. I agreed with the doctor that because of its upkeep and the potential for infection, we wanted the
Shortly after we arrived, I went to the nurses’ station to see Jennifer. She said that she had been waiting for me to arrive so that I could administer Dad’s morning meds. At practically the same time, Dr. Smith arrived and we discussed Dad’s feeding tube and his invasive lines. I agreed with the doctor that because of its upkeep and the potential for infection, we wanted the  I returned to the hospital at 2:00 P.M. to find that Jennifer and the aide were giving Dad a bath. When they were finished, Jennifer and I maneuvered Dad into the wheelchair. Jennifer thought that he was a bit weaker than yesterday and said that she wanted him back in bed in about an hour. It was a nice day, so after I had Dad cough up some secretions, we headed outside in the wheelchair. We strolled on all of the available sidewalks, which still wasn’t much of an outing, and then settled under the covered hospital entrance. While we were sitting out front, Stan and Mom drove up and visited. Stan could stay for only a couple of minutes because they had been grocery shopping and he had to get the perishables home. Mom and I visited outside with Dad until 3:25 P.M. Shortly after the three of us returned to Dad’s room, Jennifer, Hector, and I put him back in bed. Mom and I visited with Dad until about 4:30 P.M.
I returned to the hospital at 2:00 P.M. to find that Jennifer and the aide were giving Dad a bath. When they were finished, Jennifer and I maneuvered Dad into the wheelchair. Jennifer thought that he was a bit weaker than yesterday and said that she wanted him back in bed in about an hour. It was a nice day, so after I had Dad cough up some secretions, we headed outside in the wheelchair. We strolled on all of the available sidewalks, which still wasn’t much of an outing, and then settled under the covered hospital entrance. While we were sitting out front, Stan and Mom drove up and visited. Stan could stay for only a couple of minutes because they had been grocery shopping and he had to get the perishables home. Mom and I visited outside with Dad until 3:25 P.M. Shortly after the three of us returned to Dad’s room, Jennifer, Hector, and I put him back in bed. Mom and I visited with Dad until about 4:30 P.M. Stan and I stayed up late to watch the total lunar eclipse (blood moon). While watching the moon, my dear friend Rhoda texted me to see how I was doing. I quickly called her to let her know about the miracle and our change in plans.
Stan and I stayed up late to watch the total lunar eclipse (blood moon). While watching the moon, my dear friend Rhoda texted me to see how I was doing. I quickly called her to let her know about the miracle and our change in plans.
 I practically ran back to Dad’s room to tell Mom the good news. Marty stopped by a few minutes later at 2:00 P.M. and asked if we wanted to review some brochures for Home Care providers. We knew that Adan worked for Scott & White Home Care and worked with the physical and occupational therapists that would care for Dad. Ironically, our decision to go with
I practically ran back to Dad’s room to tell Mom the good news. Marty stopped by a few minutes later at 2:00 P.M. and asked if we wanted to review some brochures for Home Care providers. We knew that Adan worked for Scott & White Home Care and worked with the physical and occupational therapists that would care for Dad. Ironically, our decision to go with  Dad was a little tired after dialysis and didn’t feel up to much physical therapy. He didn’t get out of bed but did agree to some exercises in bed. Shortly after Jennifer left Dad’s room, Mom started feeling very lightheaded and faint. I got her a glass of water and I had Dana, the nurse, check her pulse. It was 82, which was fine, but Mom’s lightheadedness didn’t go away. While I watched this unbelievable mini-drama play out, I noticed Dad’s razor sharp focus on Mom that never wavered. I felt like an intruder on an intimate moment. I then asked Dana to take Mom’s blood pressure. Her blood pressure was very high, and the nurses strongly suggested that I take her to the emergency room at Memorial. I couldn’t believe it, and myriad emotions washed over me. Just minutes earlier we had been so elated about Dad, and now I was very worried about my mother. What was it with my parents and their dueling maladies? The nurse fetched a wheelchair while I pulled the car to the front entrance and we drove five miles to Memorial.
Dad was a little tired after dialysis and didn’t feel up to much physical therapy. He didn’t get out of bed but did agree to some exercises in bed. Shortly after Jennifer left Dad’s room, Mom started feeling very lightheaded and faint. I got her a glass of water and I had Dana, the nurse, check her pulse. It was 82, which was fine, but Mom’s lightheadedness didn’t go away. While I watched this unbelievable mini-drama play out, I noticed Dad’s razor sharp focus on Mom that never wavered. I felt like an intruder on an intimate moment. I then asked Dana to take Mom’s blood pressure. Her blood pressure was very high, and the nurses strongly suggested that I take her to the emergency room at Memorial. I couldn’t believe it, and myriad emotions washed over me. Just minutes earlier we had been so elated about Dad, and now I was very worried about my mother. What was it with my parents and their dueling maladies? The nurse fetched a wheelchair while I pulled the car to the front entrance and we drove five miles to Memorial.
 We met with the representative from Scott & White and although she seemed very professional and they would provide a good service, we were sick and tired of this organization and wanted to cut our ties with them. I confess that I entered the interview with a somewhat closed mind and I didn’t note the name of the person whom we interviewed. I wish that I had because I owe her a debt of thanks. Knowing that we would need some very expensive assistance, she gave us the name of a company that provided 24×7 care. The company was
We met with the representative from Scott & White and although she seemed very professional and they would provide a good service, we were sick and tired of this organization and wanted to cut our ties with them. I confess that I entered the interview with a somewhat closed mind and I didn’t note the name of the person whom we interviewed. I wish that I had because I owe her a debt of thanks. Knowing that we would need some very expensive assistance, she gave us the name of a company that provided 24×7 care. The company was  Before she left the CCH yesterday, Mom left her cell phone with Dad so that he could call her if necessary. He called her early in the morning to see if she was awake. He then called her later in the morning to tell her that someone had broken his electric shaver. He could be a pill with a phone.
Before she left the CCH yesterday, Mom left her cell phone with Dad so that he could call her if necessary. He called her early in the morning to see if she was awake. He then called her later in the morning to tell her that someone had broken his electric shaver. He could be a pill with a phone.
 When I arrived, I met Dr. Ciceri and he explained to me that Dad had something that sounded like “the Canada fungus.” He said that they planned to replace his dialysis catheter and his PIC line. The doctor had also started Dad on an antifungal. He said that he requested a TTE (transthoracic echocardiogram) for later today. I didn’t understand the significance of most of what he said, but I clearly understood what he said next. He said that Dad’s prognosis was extremely poor, that he probably had one to two months to live, and would most likely die in a nursing home.
When I arrived, I met Dr. Ciceri and he explained to me that Dad had something that sounded like “the Canada fungus.” He said that they planned to replace his dialysis catheter and his PIC line. The doctor had also started Dad on an antifungal. He said that he requested a TTE (transthoracic echocardiogram) for later today. I didn’t understand the significance of most of what he said, but I clearly understood what he said next. He said that Dad’s prognosis was extremely poor, that he probably had one to two months to live, and would most likely die in a nursing home. At 9:40 P.M., I was awakened by the house phone, and I ran to answer it before it woke Mom. As far as we were concerned, there was nothing worse than a nighttime phone call. My parents’ phone system had an audio caller ID. My heart practically stopped when I heard it announce that the call was from Scott & White. The call was from Jeliza, Dad’s nurse. According to her, Dad insisted that he wanted to go home and that he had seen Mom in the hall. He kept calling out for her, and the nurse couldn’t calm him. She hoped that my mother or I might be more successful. Jeliza held up the phone to Dad’s ear while I explained to him that we had been in his room until 6:00 P.M., but that he had been asleep. He asked me when we would return to see him again, and when I said, “tomorrow,” he asked if we’d come by early. When I told him that we’d see him after dialysis, he said that he wasn’t going to dialysis anymore and that he would go someplace else. I explained that going someplace else would require advance planning and that we couldn’t make alternative plans on a Sunday night. I promised him that Mom and I would be there and that I’d visit with him before I left for Houston. He agreed to that plan and we said good night. The nurse took back the phone and thanked me for talking with him.
At 9:40 P.M., I was awakened by the house phone, and I ran to answer it before it woke Mom. As far as we were concerned, there was nothing worse than a nighttime phone call. My parents’ phone system had an audio caller ID. My heart practically stopped when I heard it announce that the call was from Scott & White. The call was from Jeliza, Dad’s nurse. According to her, Dad insisted that he wanted to go home and that he had seen Mom in the hall. He kept calling out for her, and the nurse couldn’t calm him. She hoped that my mother or I might be more successful. Jeliza held up the phone to Dad’s ear while I explained to him that we had been in his room until 6:00 P.M., but that he had been asleep. He asked me when we would return to see him again, and when I said, “tomorrow,” he asked if we’d come by early. When I told him that we’d see him after dialysis, he said that he wasn’t going to dialysis anymore and that he would go someplace else. I explained that going someplace else would require advance planning and that we couldn’t make alternative plans on a Sunday night. I promised him that Mom and I would be there and that I’d visit with him before I left for Houston. He agreed to that plan and we said good night. The nurse took back the phone and thanked me for talking with him.
 Mom and I arrived at the
Mom and I arrived at the 
 Every morning, the doctor, nurses, or both, performed a short assessment of Dad’s mental status. From the third week after he entered the Scott & White system, he had been unable to tell the medical providers the name of the president of the United States. Although there might have been a few days in which he couldn’t remember, I suspect that most of the time he was being stubborn. He wasn’t a fan of President Obama and forgetting his name was a personal protest of Dad’s. I sometimes wondered if his refusal to acknowledge the president affected the assessment of his mental status.
Every morning, the doctor, nurses, or both, performed a short assessment of Dad’s mental status. From the third week after he entered the Scott & White system, he had been unable to tell the medical providers the name of the president of the United States. Although there might have been a few days in which he couldn’t remember, I suspect that most of the time he was being stubborn. He wasn’t a fan of President Obama and forgetting his name was a personal protest of Dad’s. I sometimes wondered if his refusal to acknowledge the president affected the assessment of his mental status.