 Wednesday, July 22, 2015: 3:45 P.M. I had just left a meeting at work and listened to the voicemail that my mother left 40 minutes earlier. “Melody, it’s Mom. I’m at the hospital with Dad and he’s not doing too well. He had a bad coughing spell during dialysis and they’re trying to bring his blood pressure down, but he’s got the shakes and delusions and all kinds of stuff. Call me on my cell, because I’m not going to leave him. Talk to you later. Bye-bye.”
Wednesday, July 22, 2015: 3:45 P.M. I had just left a meeting at work and listened to the voicemail that my mother left 40 minutes earlier. “Melody, it’s Mom. I’m at the hospital with Dad and he’s not doing too well. He had a bad coughing spell during dialysis and they’re trying to bring his blood pressure down, but he’s got the shakes and delusions and all kinds of stuff. Call me on my cell, because I’m not going to leave him. Talk to you later. Bye-bye.”
A tingly feeling crept up my neck and face, and I hoped that she was overreacting.
Earlier that day, Dad was wheeled to the dialysis room on the second floor of the CCH. His WBC count had been holding steady at 5.6, but his creatinine level was still elevated. His stubborn creatinine levels prompted his nephrologist to predict that Dad was likely to remain dialysis dependent, news that we didn’t want to hear. During his morning rounds, Dr. Anderson found Dad to be awake and alert and said that his vitals were good.
At 10:30 A.M. Dad starting coughing hard during dialysis and couldn’t seem to stop. His condition seemed to worsen immediately. Dialysis was stopped and Dad was returned to his room. Dad’s oxygen saturation levels bounced between 75% and 90%. He was coughing and suctioning large amounts thin, clear looking secretions. Michelle, Dad’s nurse, said that he was alert and had a productive cough, but it was obvious to her that Dad was in distress. The respiratory therapist was summoned to Dad’s room. She removed the red cap from Dad’s trach tube and placed him on BIPAP with 40% oxygen—a big medical and psychological step backward.
Rachel, the nurse practitioner was called to Dad’s room to evaluate his condition, and she thought that his cough appeared to be calming down. Shortly thereafter, the nurse notified Dr. Anderson that Dad’s heart rate had elevated to 150. In addition, his clear-looking secretions changed and now appeared to be Nepro. His tube feed had been stopped in dialysis when he started coughing, so they were now certain that he had aspirated his tube feed during his coughing jag. Nepro in the lungs pretty much triggers pneumonia immediately. This would be the second time that he had had pneumonia in less than three months.
On dialysis days, Mom usually arrived at the CCH around 11:30 A.M., about 10 minutes before she anticipated Dad’s return to his room. When she arrived today, she was startled to see that not only was Dad already there, the room was also teaming with activity. Michelle briefly apprised Mom about what had happened, but Mom didn’t get the impression that Dad’s condition was dire. She watched the nurses administer some meds, prop up Dad in bed, and leave the room. From what Mom could tell, it didn’t seem like the meds or the upright position did anything to improve his situation.
A short time later, Dr. Anderson told Mom that they would move Dad to a larger room next to the nurses’ station so that they could more closely monitor and attend to him. After they moved him, Mom sat in his room, watching the constant flow of nurses while they injected one medicine after another into his IV. Several times she was asked to leave his room, although she didn’t always know why.
After sitting in Dad’s room for a couple of hours, Mom called her friend Marilyn. Being the good friend that she is, Marilyn dropped everything and went to the CCH to sit with my mother. Shortly after Marilyn arrived, my mother called me and left the ominous message on my voicemail. When I returned her call at 3:45 P.M., she was very concerned, and although they had just moved Dad from BIPAP to full ventilation, she was still not convinced that I should drive to Temple before the weekend.
Marilyn and Mom sat together in Dad’s room for a couple of hours. During that time, Dad’s condition had not improved and Mom became worried. To her, it seemed like they kept trying medications but to no avail. As Marilyn and my mother talked, Marilyn asked Mom if she should call Pastor Don, but Mom didn’t know how to contact him. Marilyn was pretty active in another United Methodist Church. She didn’t have Don’s contact information, but she knew someone who did.
Pastor Don’s mobile phone rang just as he and his wife, Wynn, started eating dinner at a local restaurant. Don promised to stop by the CCH as soon as they finished dinner. Mom called me again at 5:30 P.M., and said that she wanted me to come to Temple that night. Stan had come home for dinner and was about to return to his office for the night. His birthday was becoming memorable, but not for the reasons we wanted. I had already packed a bag in anticipation of Mom’s call, but decided to wait a couple of hours before leaving. Anyone familiar with U.S. 290 would understand why I didn’t want to brave that highway until after 7:00 P.M. I said good-bye to Stan, and he said that he’d come up to Temple in a couple of days.
Between Mom’s call to me and when I left Houston, Pastor Don and Wynn arrived at the CCH. Mom and Don spent some time together in the small chapel at the CCH, and Mom said that Don was wonderful and encouraging. Finally, at 9:30 P.M., Mom, Marilyn, Don, and Wynn left the CCH.
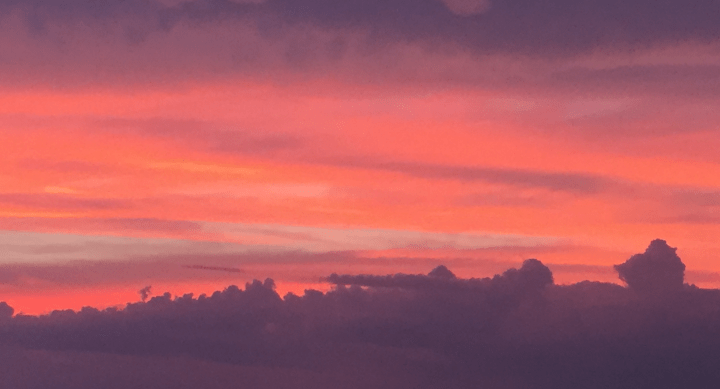
My drive west on U.S. 290 was a little surreal. The sunset was a spectacular display of stunning shades of orange. I was torn between appreciating the beauty of nature and praying that my father wouldn’t die on my husband’s birthday. I arrived at the CCH around 10:00 P.M., and made my way to Dad’s room. When I arrived, he was fully ventilated and surrounded by ice and fans in an attempt to bring down his temperature. I was met by his night nurse, Christine. She had arrived at 7:00 P.M., and was stunned by his sudden change. She told me that he had been doing pretty well, and she really enjoyed joking around with him during her shift. He had never spoken about her to me, but he’s a big kidder and it seemed like they had developed a friendly banter.
I went to his bedside and held his hand, but he didn’t know that I was there. Christine asked me under what circumstances I would want to be called during the night. I told her to consider her own father and the circumstances under which she would want to receive a call, and then I left. I had called my mother when I arrived at the CCH and she was waiting for me to arrive at the house. We were both exhausted, yet keyed up on nervous energy. We talked for a while before going to bed.
At 3:30 A.M., the phone rang and it was Michael, a nurse from the CCH. He mumbled something about how they were adjusting Dad’s medication. I listened for a moment, said “OK,” and then hung up. After the call, I wasn’t really sure why he had called. It was unsettling and confusing. I wished that I had been more alert. I learned later that he had called to tell me that my father’s condition had worsened and that Dad required additional medication and that they were going to insert an arterial line so that they could monitor his blood gases. He had probably told me that in some jargon that I couldn’t understand—especially at 3:30 A.M. Scarier still was that this phone call was to obtain consent for the procedure. About an hour later, Dad’s blood pressure dropped to 65/39, his respiration was 35, his extremities were cold, and he still had a slight fever. With full ventilation, his oxygen saturation was only 90%.
At 5:30 A.M., the phone rang again. This time it was Dr. Anderson. He told me that my father wasn’t doing well, and among a list of problems, he was pretty sure that Dad had had a heart attack during the night. He then said that they could keep on doing what they had been doing, and my father would probably die in 1-2 hours, or they could send him over to Memorial. Dr. Anderson went on to say that considering my father’s age and “extremely poor prognosis,” he assumed that we would not want to take “aggressive measures.”
God help me; I took a deep breath, and in that moment I flashed back to several conversations I had had with Dad in which he listed conditions in which he would not want to live or treatments that he would not want to endure. I told the doctor that I would call him back in a couple of minutes. I then woke my mother with the news from Dr. Anderson. I was relieved when she said, “We have to do whatever we can to help Daddy.” I immediately called the CCH and told Dr. Anderson to send my father to Memorial. He hesitated for a moment and said OK, but it sounded more like a question than an affirmation.
At 6:15 A.M., my father was moved to a stretcher and transported back to Scott & White Memorial to MICU. Following Dr. Anderson’s call, the clock seemed like our biggest enemy.

3 thoughts on “And the nightmare begins again”