August 12, 2015. Mom and I arrived at Dad’s room at 7:45 A.M. Dad was on a four-hour conventional dialysis trial to judge his tolerance. I freaked out when I saw that his feet were elevated above his head. During dialysis, patients who suffer from hypotension often have their feet elevated above their heads to their increase blood pressure. With his history of aspiration, that practice could not be applied to him. Olga, his nurse and the one who had elevated his feet, responded to my outburst and raised his head.
After Olga had repositioned Dad, I asked her about his morning lab results. I was thrilled to learn that his WBC count had dropped further and was now at 11.3. A normal WBC count seemed within sight!

Mom’s birthday was in four days, and we were anticipating that Dad would be at home when we celebrated his birthday on October 6. I thought that we should have a four-tier birthday cake on Dad’s birthday—one tier for each of the birthdays we missed celebrating this year. Dad seemed to brighten up at idea and indicated that he wanted chocolate, Mom wanted carrot cake, I wanted rum cake for my layer, and I decided that Stan wanted apple cake.
During rounds, we met the new attending physician, Dr. Shekhar Anant Ghamande. He said that Dad was progressing and that things were getting better, but that Dad needed some exercise.
Dad was a bit difficult to handle. He kept trying to talk, which was impossible, and he refused to use the letter board to communicate. Other than learning that he wanted chocolate cake for his birthday, we had no successful communication with Dad.
The conventional dialysis trial, which Dad completed without much difficulty, was over at 1:15 P.M. Dad was moved into the cardiac chair, but he would not put his feet on the chair’s foot stand. Without his feet on the foot stand to stop him from sliding off the chair, the nurse had to reposition him in the chair every few minutes. Mom left the room for a few minutes and when she returned, she heard singing coming from Dad’s room. While she had been away, a Catholic nun from the hospital’s chaplain office had stopped by to see Dad. With Dad’s refusal to use the letter board to communicate, I couldn’t imagine how they communicated.
Dad tired of sitting in the chair and wanted to get back into bed. The nurse had left the room to find someone who could help her, but while she was gone, an ultrasound tech arrived and spent about an hour checking Dad’s legs and arms. The nurse later said that by the time that the tech left the room, Dad was as inspired to transfer back into bed as she had ever seen him. We never did learn about the purpose of the ultrasound, but at least a couple of us were glad for his extra time in the chair.
When Mom and I returned to the hospital after dinner, we were pleased to see that Dad was sleeping and that Tyler was his nurse again. It was the first day in many days that I could tell Stan that we had had a good day today.
August 13. As Mom and I drove to the hospital, we realized that Dad was starting his 100th day in the Scott & White institution. We arrived at the hospital at 7:35 A.M. Dad was restrained, but I quickly removed the soft restraints.
Dad was all hot and bothered to get out of the bed at 7:45 A.M. Anna, his nurse, was pretty busy, so we had to wait until 9:45 A.M. to get him into the chair. During Dad’s initial stay in the ICU, he hated the uncomfortable chairs, and practically fought to stay in bed. Mom and I were glad that he now wanted to get out of the bed.
At 10:00 A.M., Travis and his entourage of occupational and physical therapists stopped by to exercise Dad. They stood him up from the chair and onto the floor. Dad’s legs would not straighten out, but he was able to kinda sorta stand, with some assistance. The therapists worked with him for about 10 minutes, moving his arms and legs. Cardiac chairs are designed to take patients from a recumbent to a sitting position. You don’t usually step out of or into a cardiac chair. Getting Dad resituated into the chair was a real struggle for the three therapists, but they eventually succeeded.
Mom left the room to call April Jones, the nurse manager at the CCH, to see if she could make an appointment to meet with April next week. We had not been thrilled with our previous experience with them and wanted a better relationship the next time. Mom wanted to start working on that now.
While Dad was in the chair, Michelle, the dietitian, had stopped by for one of her routine visits. In addition to her usual concerns about Dad’s nutrition, she was now concerned about the extended use of antibiotics and how they could affect his digestion. She said that she would suggest that the doctors consider starting him on probiotics. I don’t know if they ever did add probiotics to his daily regimen of meds.
After Dad got back into bed, he slept for 10 minutes and then woke up and started worrying the bed linens and pulling on his lines and trach tube. Dad seemed to be having lots of secretions, and he seemed to be struggling to breathe. Nikita, the respiratory therapist, happened to walk past the room as he was having breathing problems. She said that Dad had been on CPAP since 7:00 A.M. She thought that it was time to give his lungs a break, and switched him back to BiPAP support shortly before we left for dinner.
Mom and I returned to the hospital at 6:40 P.M., just prior to the shift change. The big pleasant surprise for us was that Andrea was Dad’s night nurse. She had been his nurse for the first three days when Dad returned to Memorial, and Mom and I loved her. When we first met her, Andrea had mentioned that she usually liked working nights, and we were glad to see her again and assigned to Dad. She commented on how much Dad had improved since she had last seen him 19 days earlier.
Mom and I stayed with Dad until about 8:00 P.M. On the way out of the hospital, we walked over to the Cardiothoracic Intensive Care Unit (CTICU) in the north tower, which was where Dad stayed during his first stint at Memorial. In addition to seeing a couple of the nurses we knew, we were enthusiastically greeted by a nurse we didn’t remember. Mom and I were really touched by the outpouring of support that we received from some of the caregivers in CTICU. Today had been another pretty good day, and we left the hospital at 8:15 P.M., feeling like Dad would have a relatively good night.

August 14. Mom and I arrived at the hospital at 7:45 A.M. to find that again Dad was restrained. Evidently, Andrea had had to restrain him about four hours earlier because he was trying to pull out his trach tube and PICC line. As I had done for the past few days, I untied Dad’s restraints. Almost immediately, Christine, his nurse, reprimanded me for removing his restraints and reminded me about the importance of restraints and notifying the nurses, and blah, blah, blah. I had a pretty good relationship with most of the nurses and caregivers, and they knew that we were a constant presence in Dad’s room. It wasn’t as if Christine had never laid eyes on us. Dad’s room was right in front of the nurses’ station. While I understood the importance of the restraints for patient safety, I was annoyed at the cavalier attitude that some nurses seemed to have about them. As far as I could tell, restraints were used because the hospital could not assign someone to watch him. Wouldn’t you think that a nurse would ask family members if they would or could stay with the patient so that they could remove the restraints? My father wasn’t unconscious; he knew that he was tied to the bed. Who in the world would think that being restrained was good for patient morale?
On a more positive note, Dad’s WBC count was down to 10.4, which was finally in the normal range; it was a tad on the high side, but normal nonetheless.

Drs. Hayek and Stewart (who I affectionately dubbed the fellows) stopped by and we discussed the status of Dad’s breathing and the possibility of having the speaking valve trial on Monday. However, before Dad could get a speaking valve, he had to be able to breathe on the trach collar. Dr. Stewart told us that the respiratory therapist would stop by later in the morning to make the switch.
It was Friday, the day we referred to as the last day of dialysis for the week. As Carlos, the dialysis nurse, was setting up the dialysis machine, Dr. Nimrit Goraya, the attending nephrologist, stopped by with her nephrology fellow and residents in tow. She told us that because Dad had tolerated the last conventional dialysis trial, he would receive another four hours of dialysis again today. Carlos got the dialysis started at 9:30 A.M. In principle, Dad’s dialysis session would be over by 1:30 P.M.
During Dad’s morning trach care, Ashley, the respiratory therapist, changed out the ventilator apparatus for a trach collar and trach mask. The trach collar test was on!
I stayed home after lunch, but Mom returned to the hospital at 1:00 P.M. Shortly after she arrived, Dad started foaming around his trachstoma. She quickly located Ashley and Dr. Stewart, who said something about a hypoxic episode. Ashley switched Dad back to the ventilator. Although Dad had failed his initial breathing test, Dr. Stewart said that it was still a good day. Unbelievably, Dad slept through the whole ordeal, and he slept for the remainder of the time that Mom was with him.
Dad’s dialysis session was over at 1:15 P.M., and they were able to remove 1,400 ml of fluid without any instances of hypotension, which moved him one step closer to being discharged from Memorial to the CCH.
I arrived at the hospital at 6:45 P.M., and once again was very pleased to see Andrea. Dad was awake and looked pretty good. However, soon after I arrived he became very agitated and wanted to get out of bed. He insisted that he needed to get out of bed to use the bathroom. I had to hold him down. He tried to push me away, but for the first time in my life, I was stronger than him. He kept edging his feet over to the side of the bed like he was trying to get up. He finally started pulling his pillow out from behind his head and indicated that he was uncomfortable. I called Andrea and told her that Dad needed to be repositioned. Andrea and another nurse respositioned him, which seemed to calm him a little and divert his attention from his original purpose. Because of his agitation and the fact that he had had to be restrained the previous two nights, Andrea also gave him some Seroquel through his feeding tube. According to Andrea, the doctor had increased Dad’s dosage of Seroquel for nights when he was restless.
I was shooed out of the room at 7:45 P.M. so that Andrea could tend to him. I probably wouldn’t have been able to come back into his room for at least 15 minutes, so it seemed like a good time to go home. Dad had been so distraught during the time that I was there that I hated leaving him, and left feeling a little conflicted. It just hadn’t felt like a good day.

 August 9, 2015. We arrived at the hospital at 9:00 A.M. to find that Dad was still asleep and restrained, the nurse’s name was not on the board, and Dad’s feeding tube was empty. Two out of three of these situations were unacceptable. I went to the nurse’s station to find out who his nurse was and to let them know that his tube feed bottle was empty. A nurse entered the room with a fresh bottle of Nepro, changed out his tubing, and replaced the empty bottle. The nurse also told me that Dad’s nurse was Nicole, who finally showed up at 9:15 A.M. and introduced herself.
August 9, 2015. We arrived at the hospital at 9:00 A.M. to find that Dad was still asleep and restrained, the nurse’s name was not on the board, and Dad’s feeding tube was empty. Two out of three of these situations were unacceptable. I went to the nurse’s station to find out who his nurse was and to let them know that his tube feed bottle was empty. A nurse entered the room with a fresh bottle of Nepro, changed out his tubing, and replaced the empty bottle. The nurse also told me that Dad’s nurse was Nicole, who finally showed up at 9:15 A.M. and introduced herself.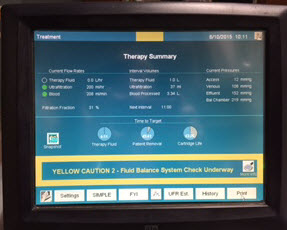 August 10. We arrived at 7:40 A.M. and noticed that Dad was already on dialysis. Before we arrived, they had drawn blood and ran an
August 10. We arrived at 7:40 A.M. and noticed that Dad was already on dialysis. Before we arrived, they had drawn blood and ran an